Value Chain
HǣlthTech is a cost-effective, highly flexible internet-based insurance system that lowers the overall cost of management of both Group Health and Group Risk products for fully insured groups or companies that are self-insured.
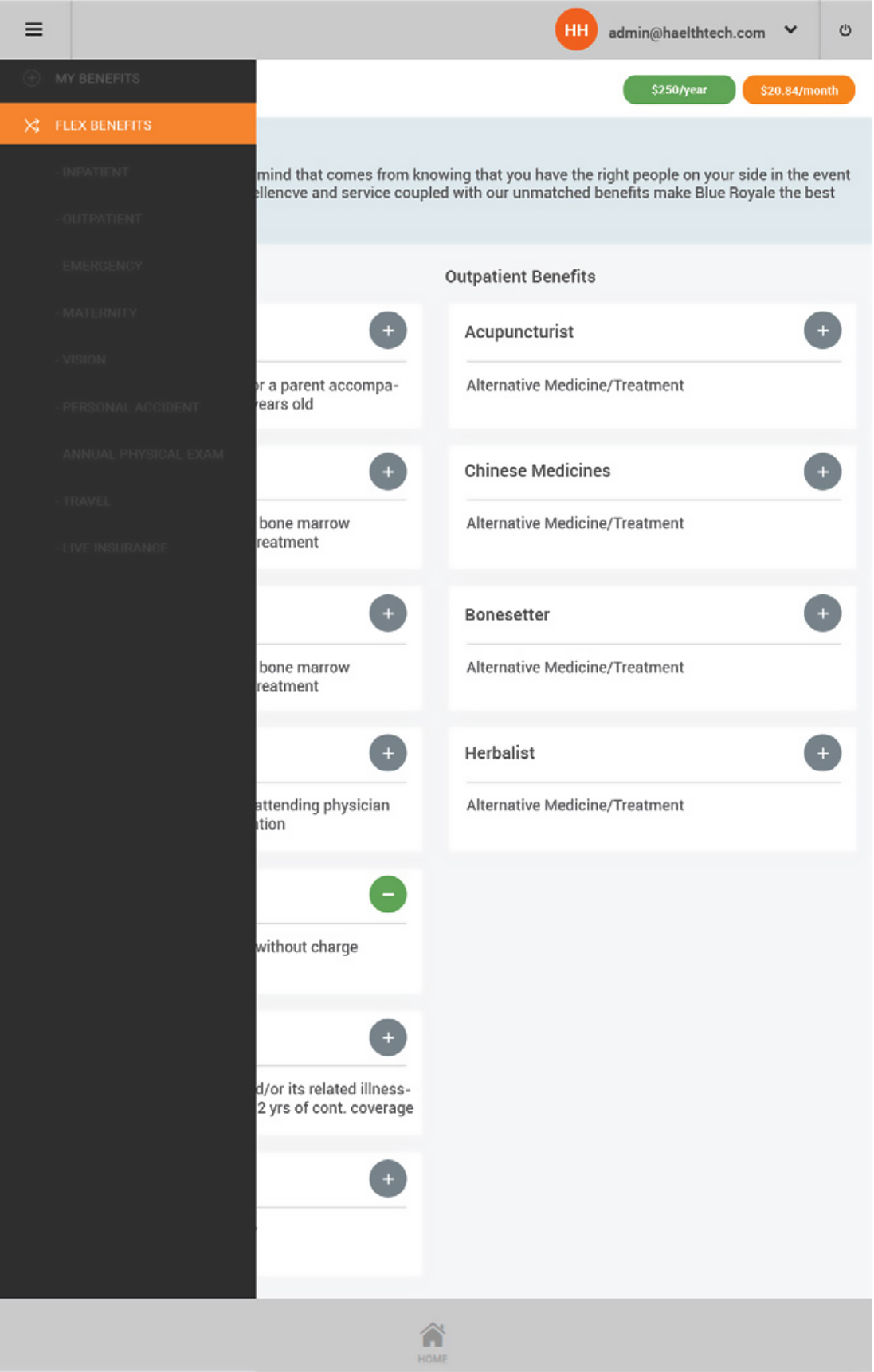
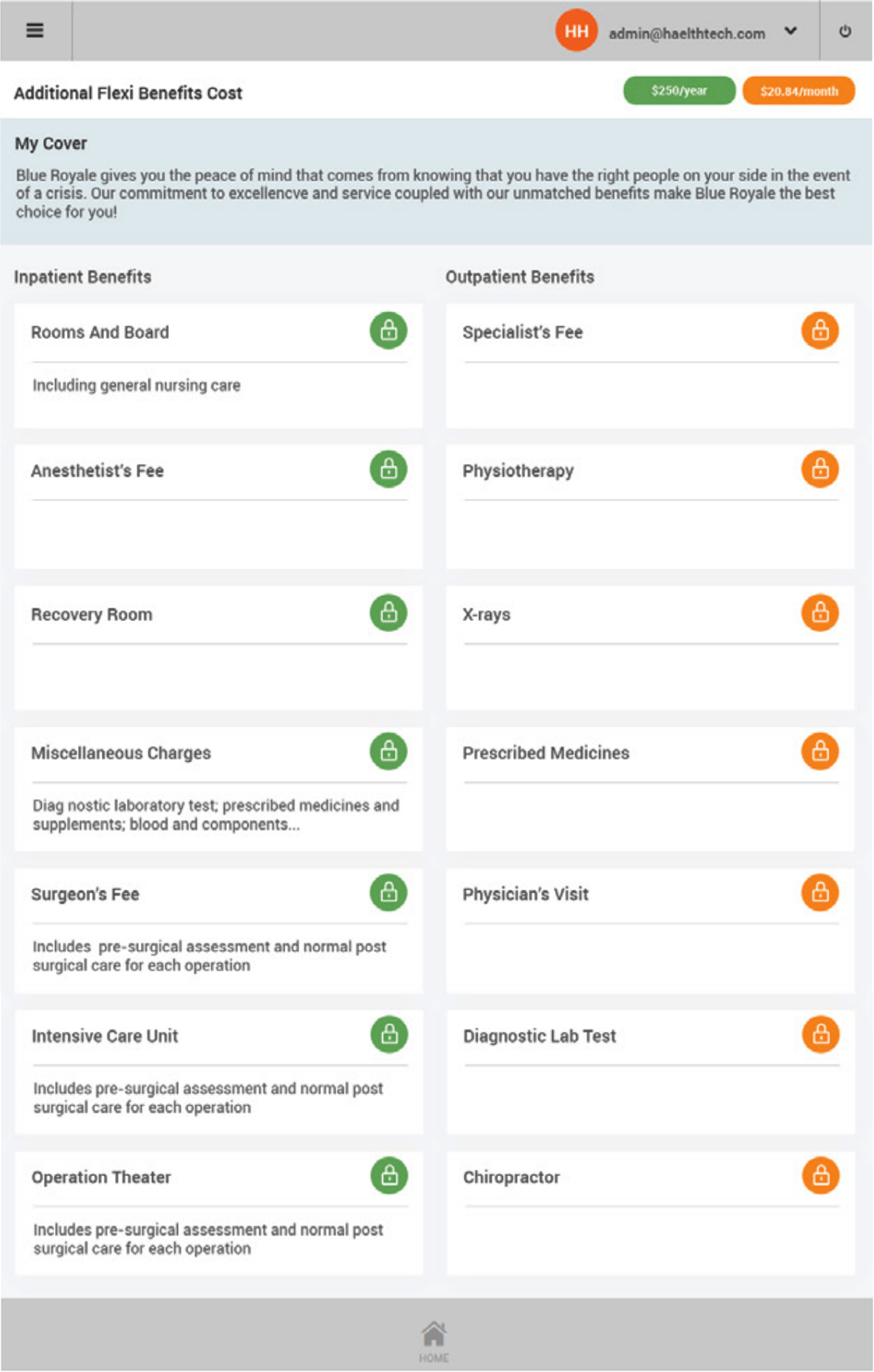
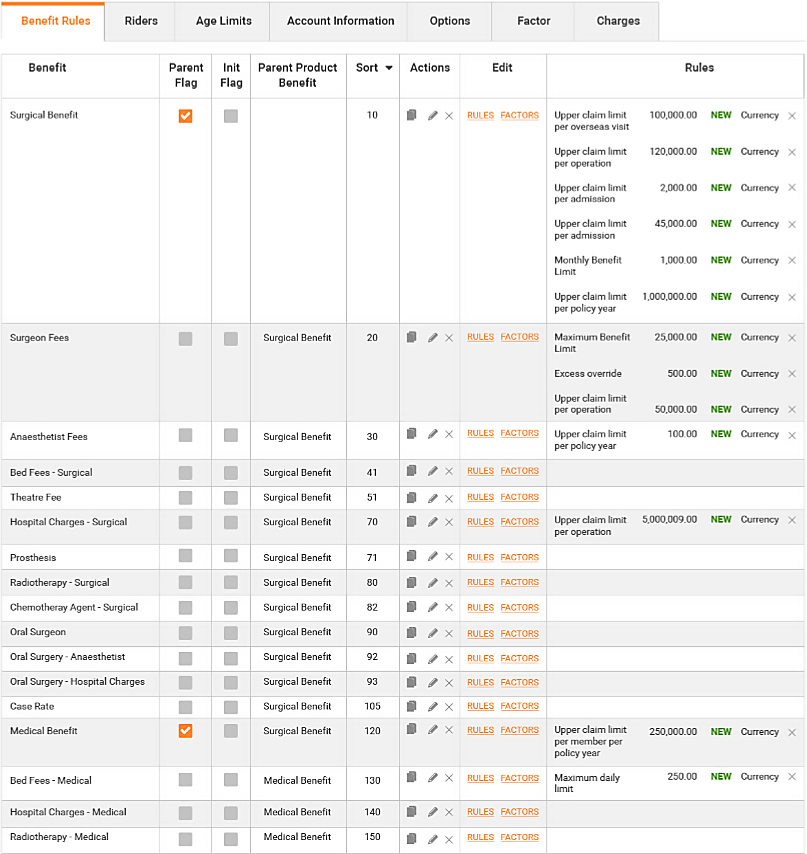
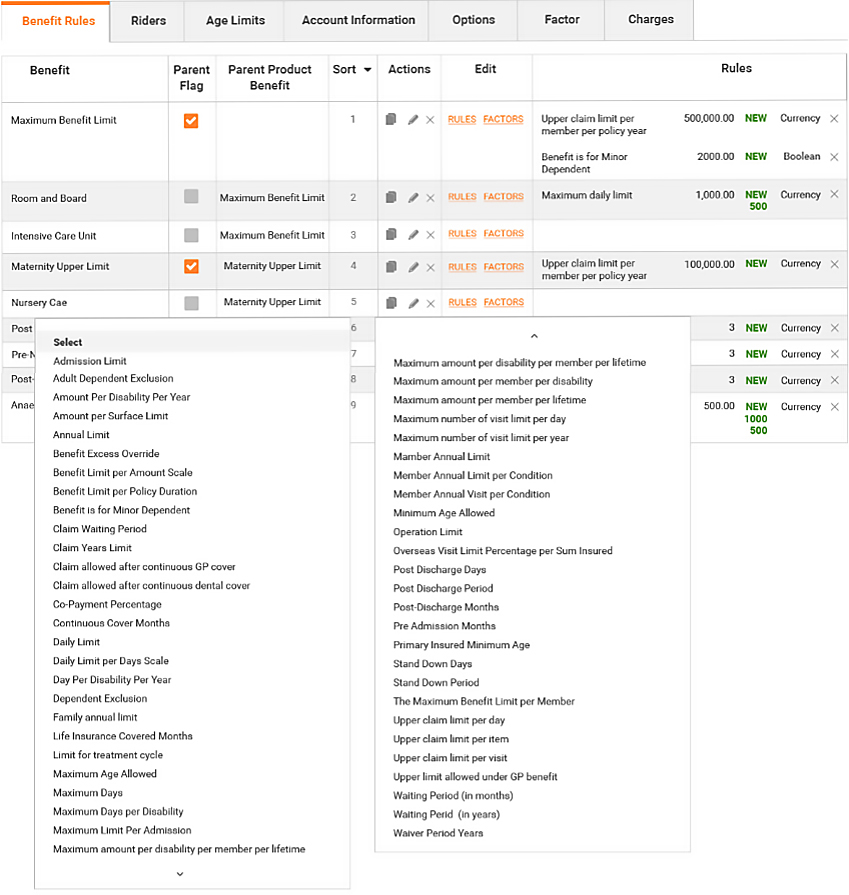
Product and benefit establishment
Complex products can be fully customized by users
- Products are defined for a particular underwriter
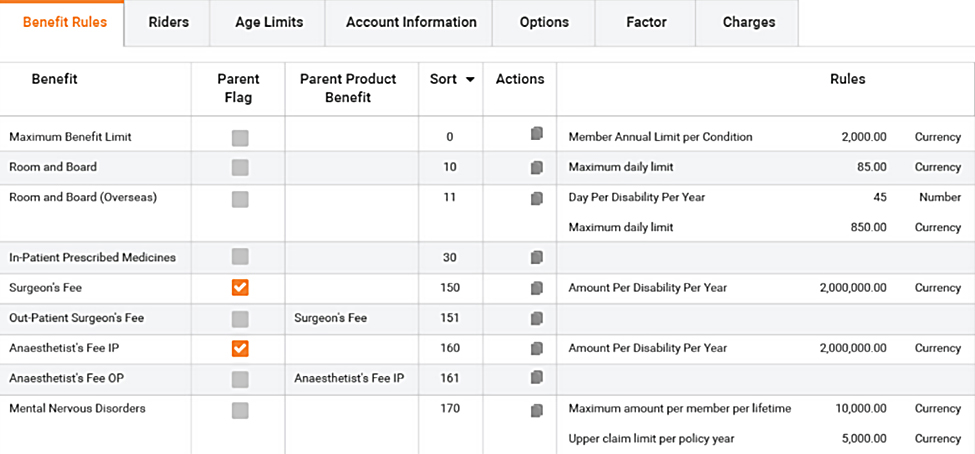
- Benefits defined with associated rules to drive automated claims adjudication and policy management
- Rate card controls premium calculation
Policy updates
Online updates of member and policy information by administrator
- Detailed audit maintained
- Ability to update member policy details including billing, receipt details, banking details for claim payments and direct debit receipts
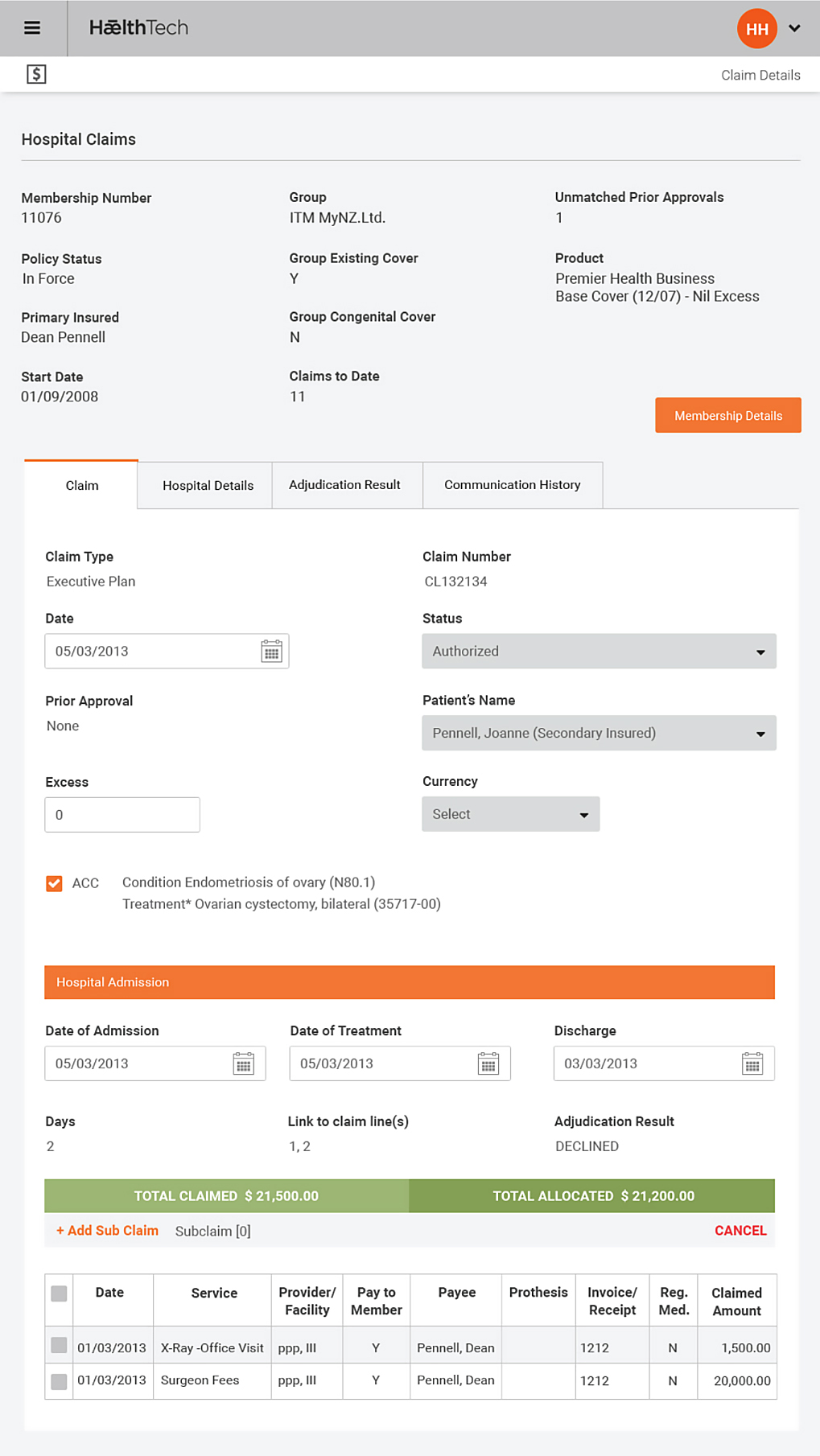
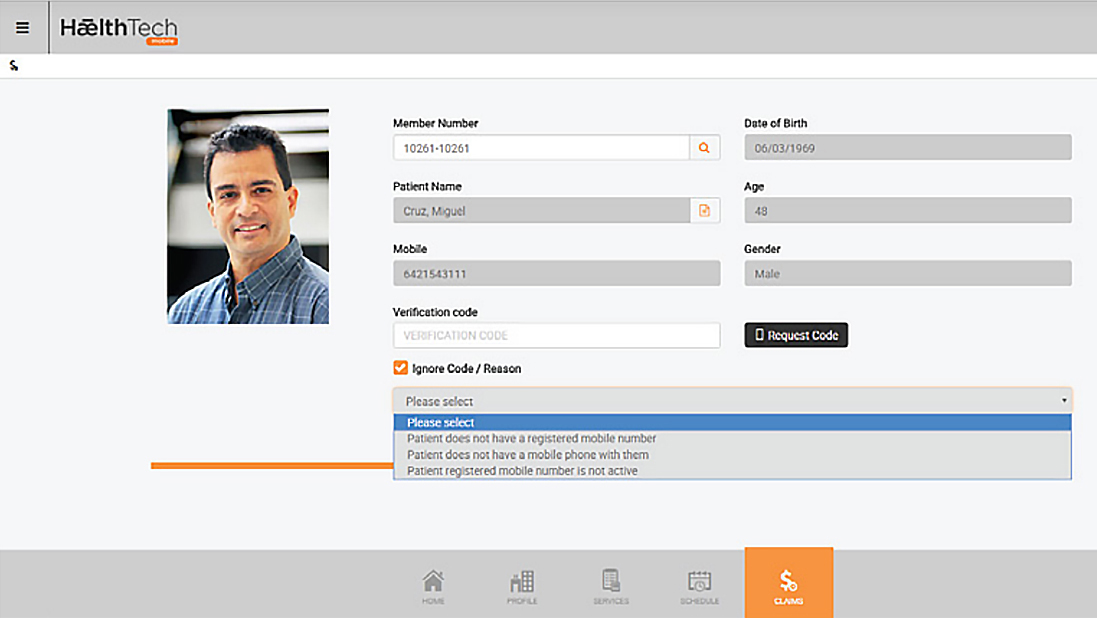
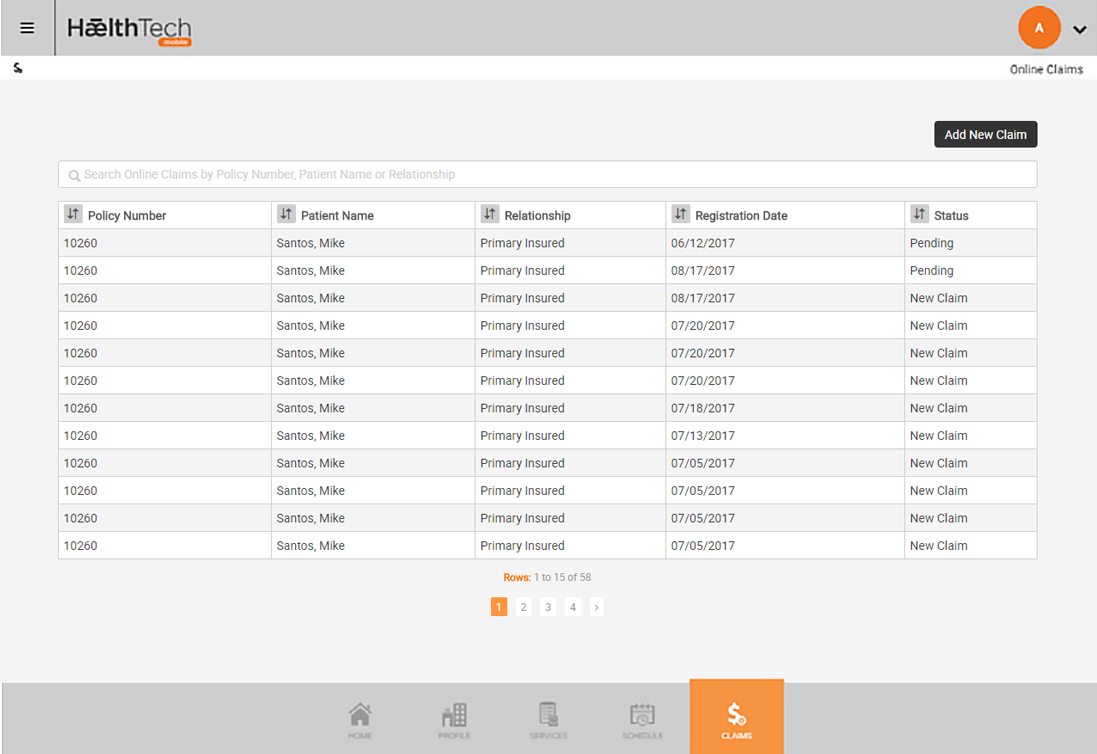
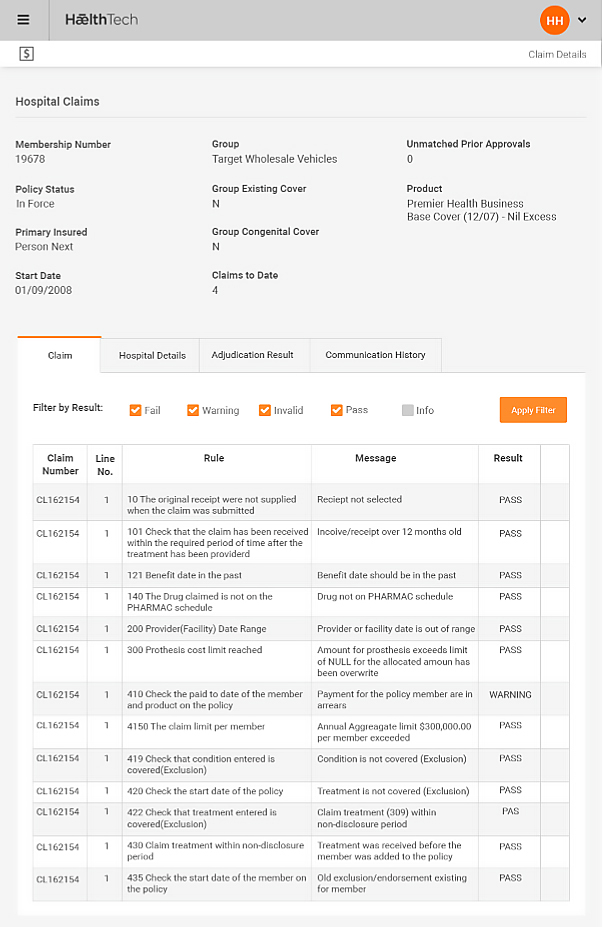
Claims Management
Manages claims and prior approvals for hospital and primary care
- Automatic claim generation from authorized prior approval
- System steps through adjudication process against a series of defined checks
- System calculates for each member and product total premium, tax, installments and risk portion based on member demographics using list of rate cards for products and underwriters
Accounts Receivable
Monitoring of group and individual Accounts Receivable
- Creates individualized overdue payment letters
- Calculates commission for ongoing payments to Vendors and can be customized for advisor management
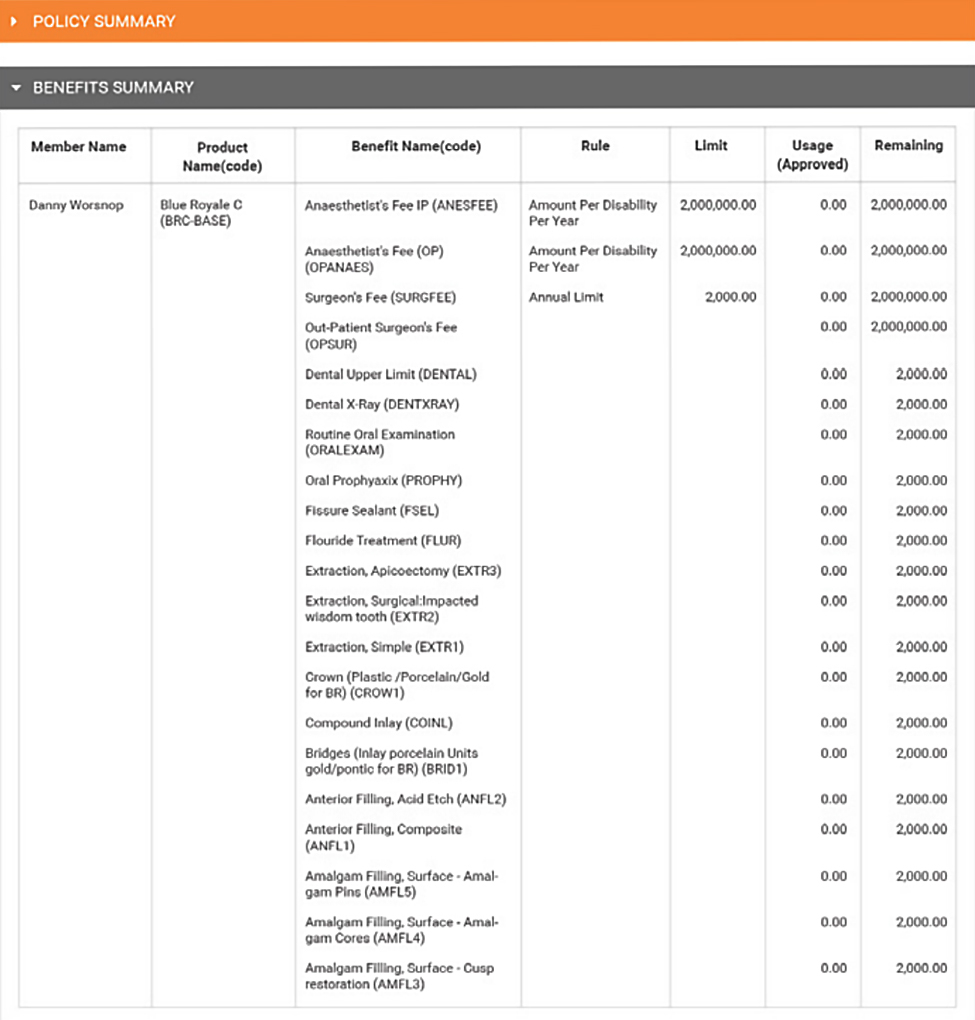
- On line review of employee information and benefits
- On line claims and updates by members
- Business intelligence and management reporting
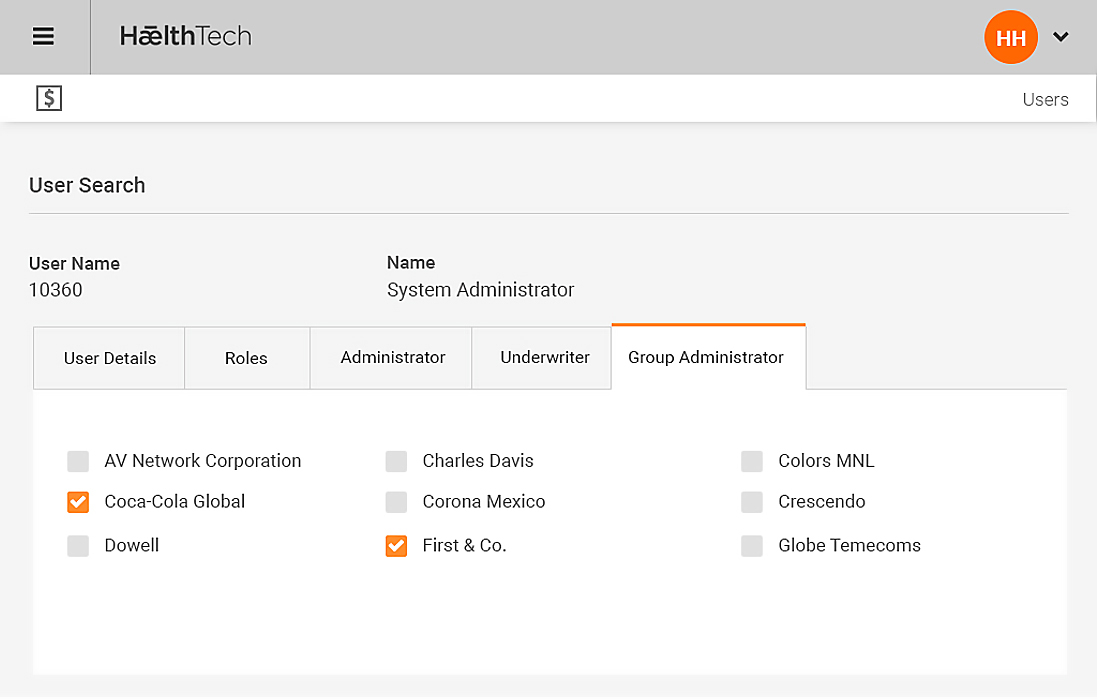
Group and Individual set up
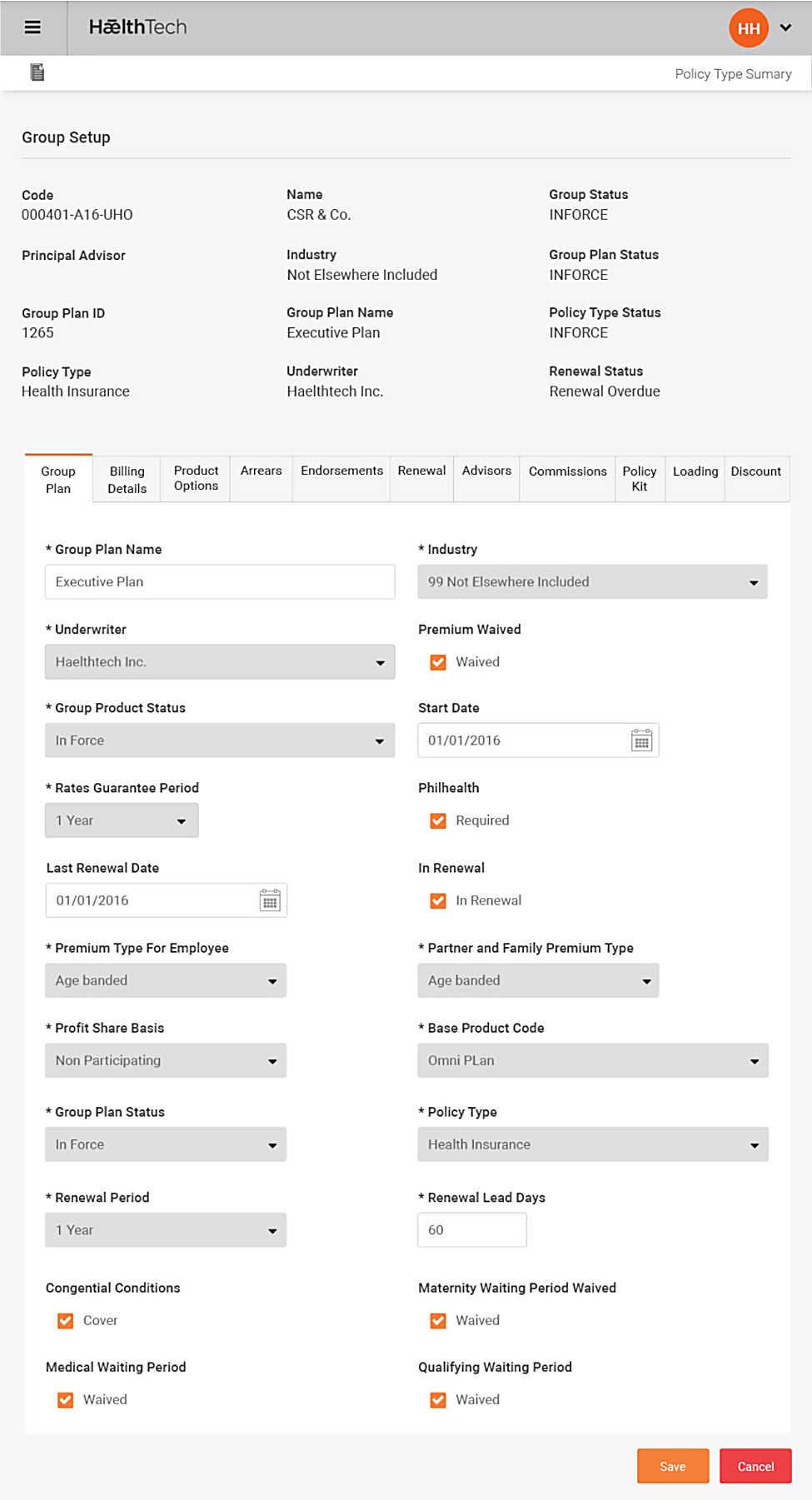
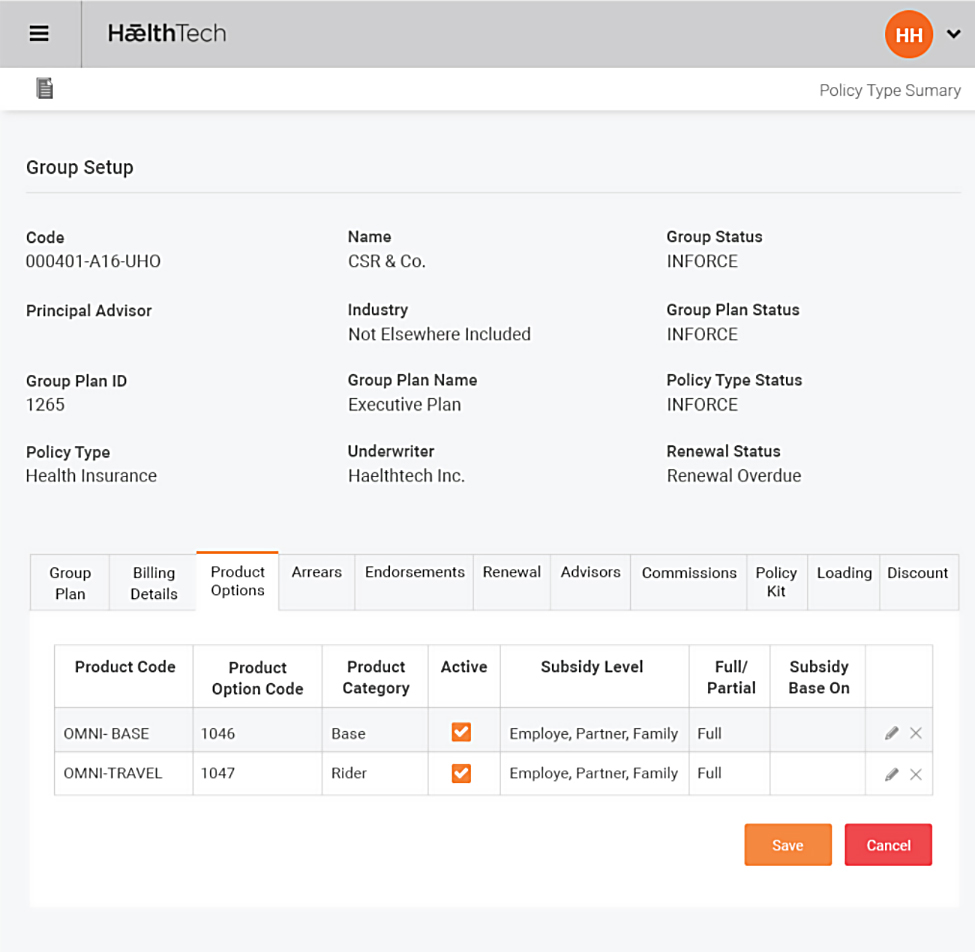
Group and Individual can be set up of different products or groups of products from different underwriters
- Easily defined groups, divisions and locations
- Assigned premium calculation methods, billing methods and frequency
- Members’ details loaded into HǣthTech using standard policy upload interface
- Automatically creates policies and calculates initial installment and annualized premium<
Multiple Underwriters
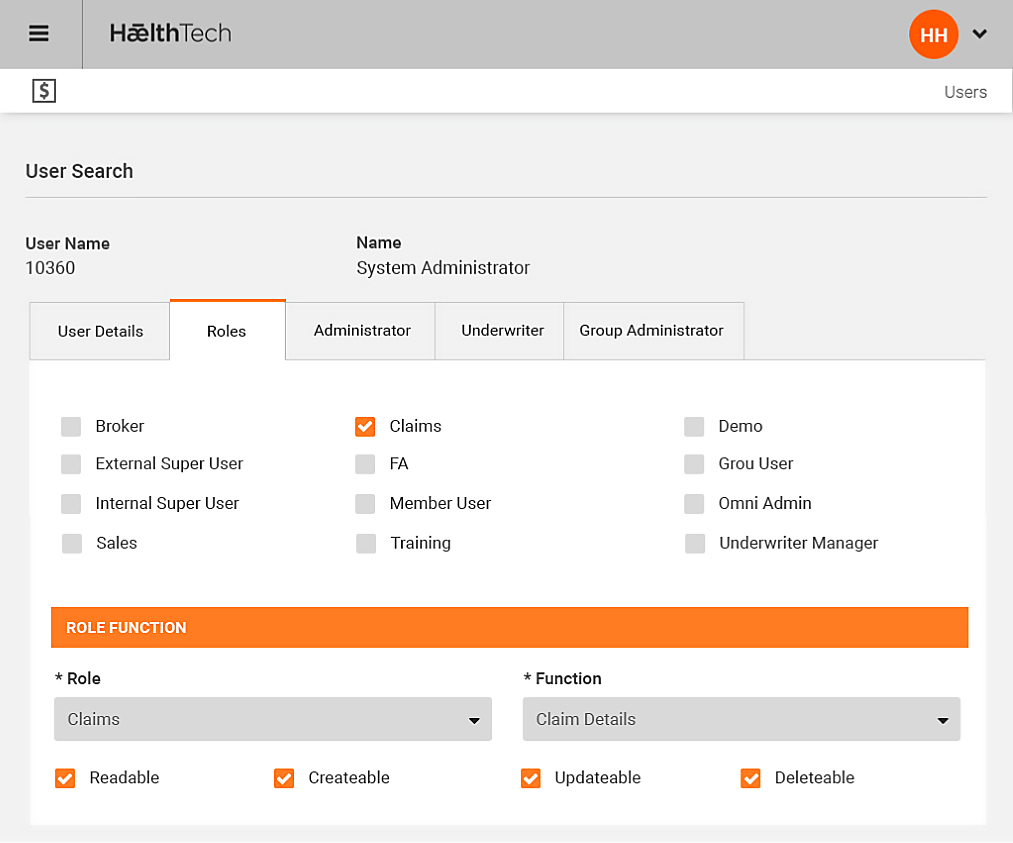
Supports multiple underwriters and for different products to be defined by an underwriter
- Security settings to limit amount of information the user wishes to provide
- Underwrite can run and download account and data warehouse extracts on line
- Underwriters can review and authorize pre-approvals, claims and medical invoices
Billing
Billing tool supplied with flexibility to cover various premium rates and frequencies from weekly to annual
- Automatic direct debits and payments matched against premiums raised
- Option to calculate credit billing and re-billing for retrospective changes to policy or premium