Mobile Solutions
The Omni Member Mobile application enables members to use mobile devices (iOS, Android) to access and transact a range of functions from Smartphones, tablets or from a computer.
Using a RAD platform to build Omni we are able to build new modules faster, decrease maintenance costs and ensure that no matter how big the change, our applications will always be architecturally sound and functional. The Platform tracks global dependencies and pinpoints the impact of a change across all layers of your application. It heals the sections that can be automatically corrected and tells you about the required manual corrections. It also automates the deployment process including all database change scripts and the impact this change will have in the running application.

Modules
Policy Details
- Policy List
- Policy Details
- Policy Members
- Schedule of Benefits
- Benefit Utilization
Chat
- Chat to provider
Claims
- My Pending Claims
- Enter a claim
- Photo and upload claim receipts
Member Products
- Product Options
- Member/Member Profile
- My Information
- View My Policies
- Edit Personal Information
- Edit Contact Information
- Edit Payment Information
- Edit My Credential
- Reference documents
- Reports
- Member Lifestyle
- Member Benefits Options
- Chatbot
References
- Policy document and wording download
- Schedule of Benefits
- Claim Form Downloads
My Appointments
- Locate a Provider
- Schedule and Appointment
Provider List
- Profile
- Services
- Specialities
- Schedules
- Claims
- Location
- Affiliates
- Coordinators
- Reference
- Reports
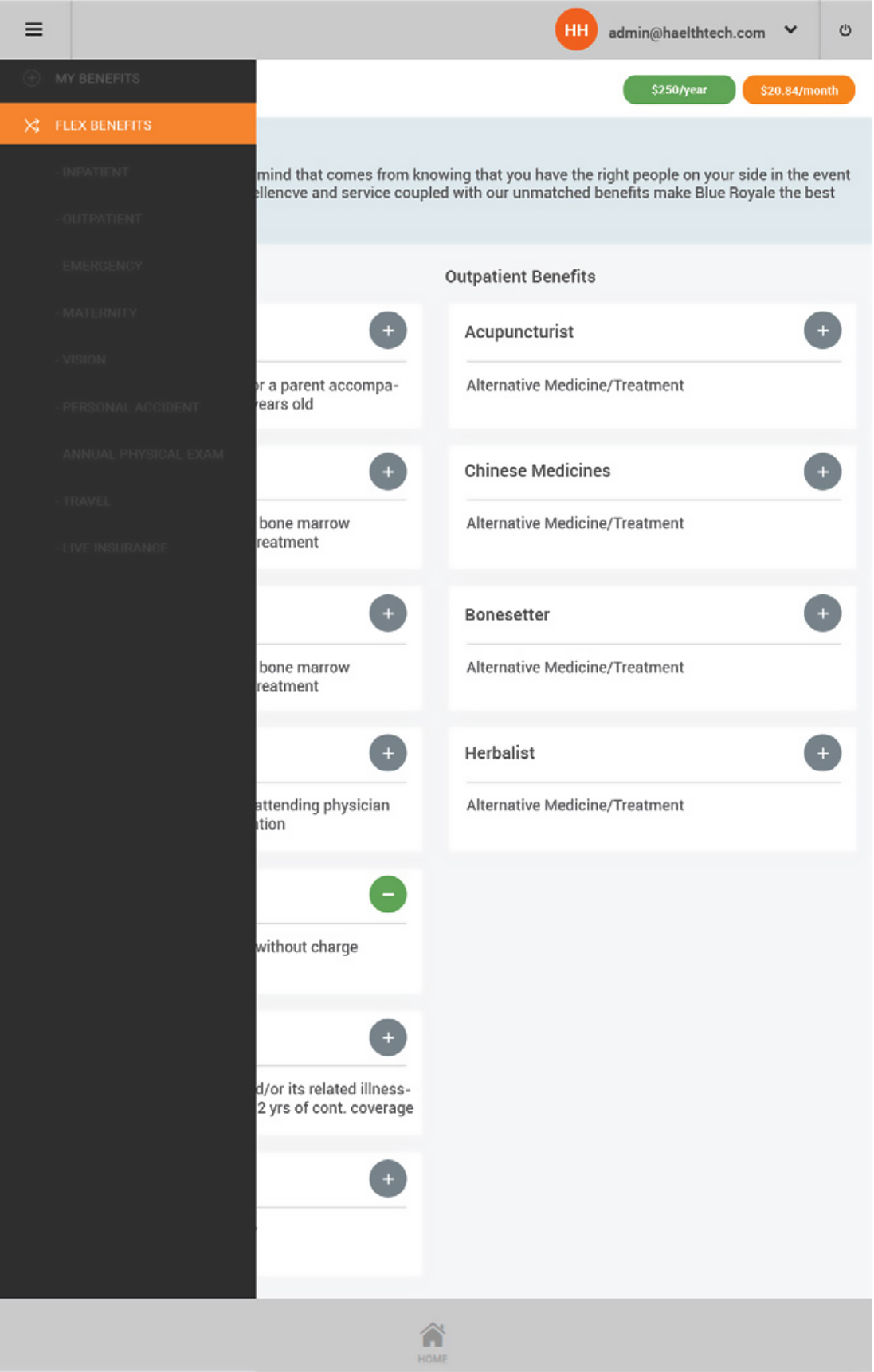
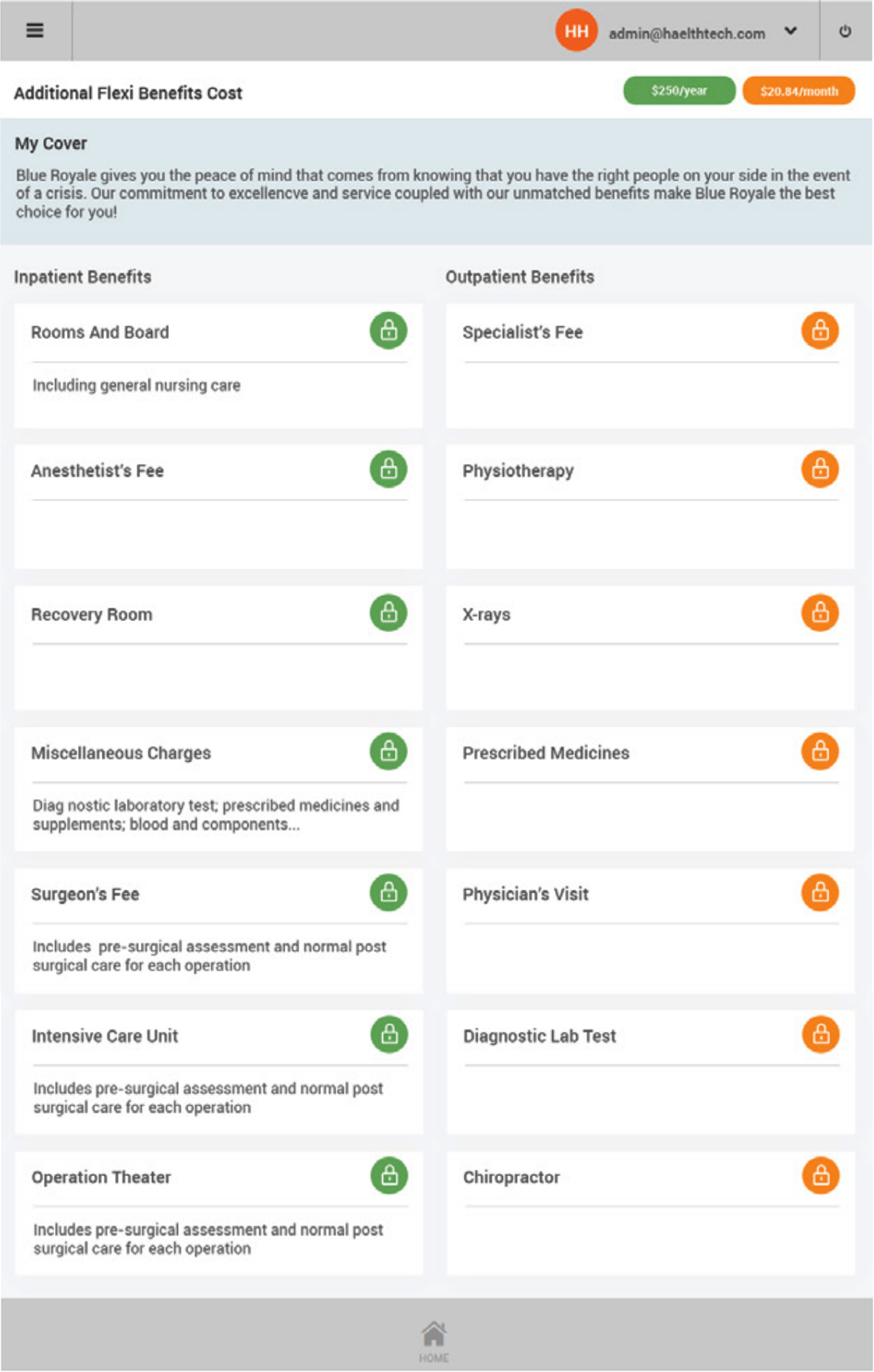
My Benefits
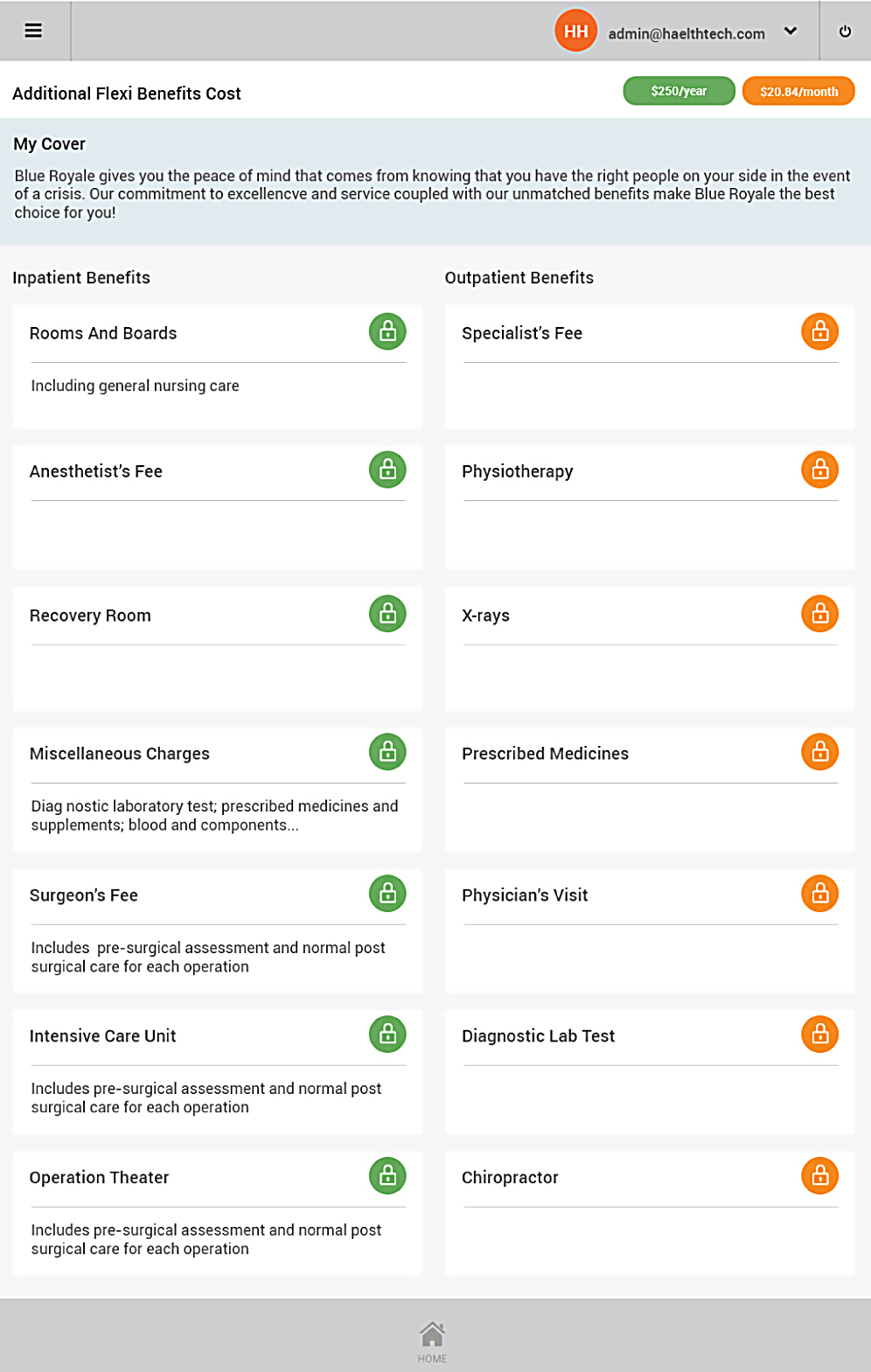
Figure 13 - Technology used to build the Omni system
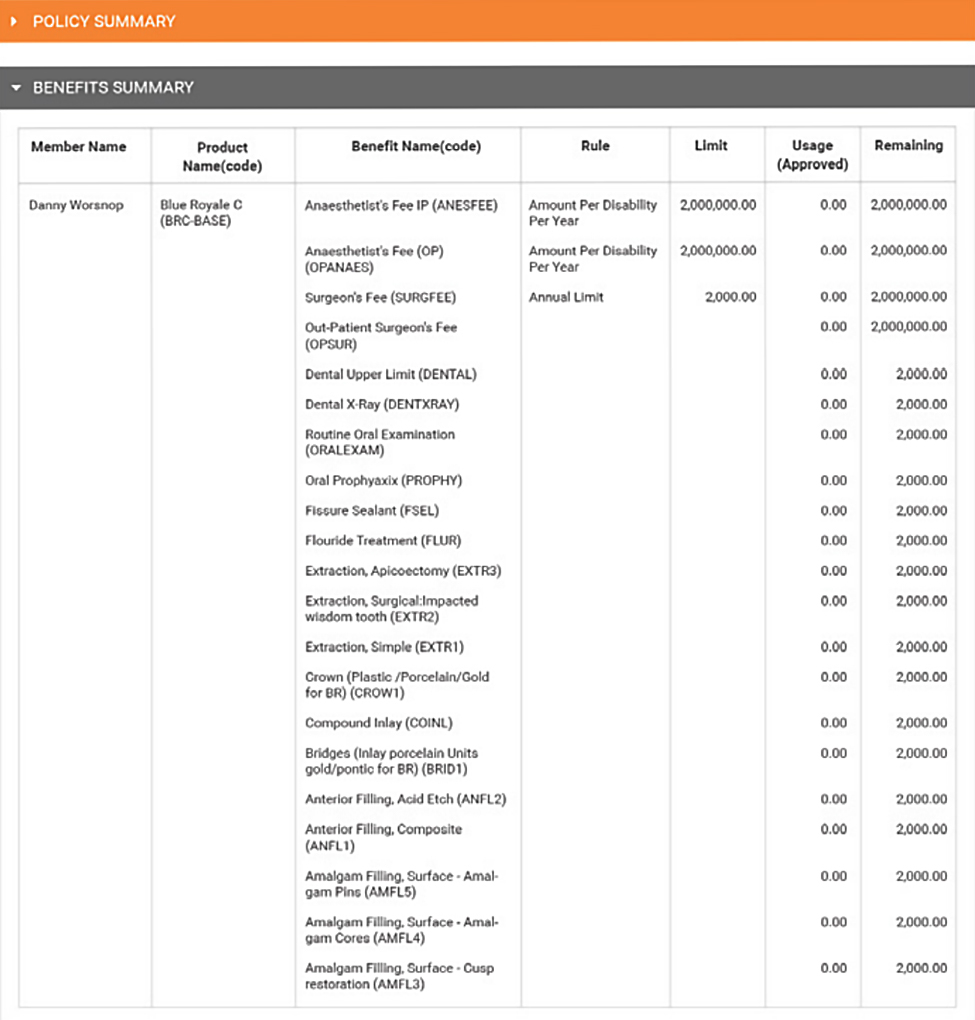
My Benefits
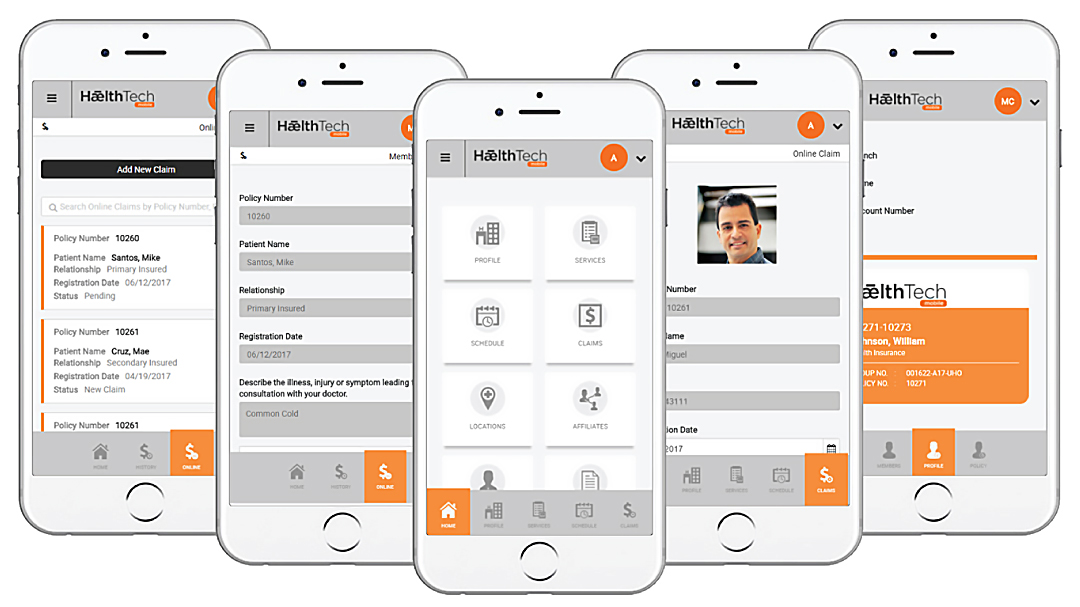
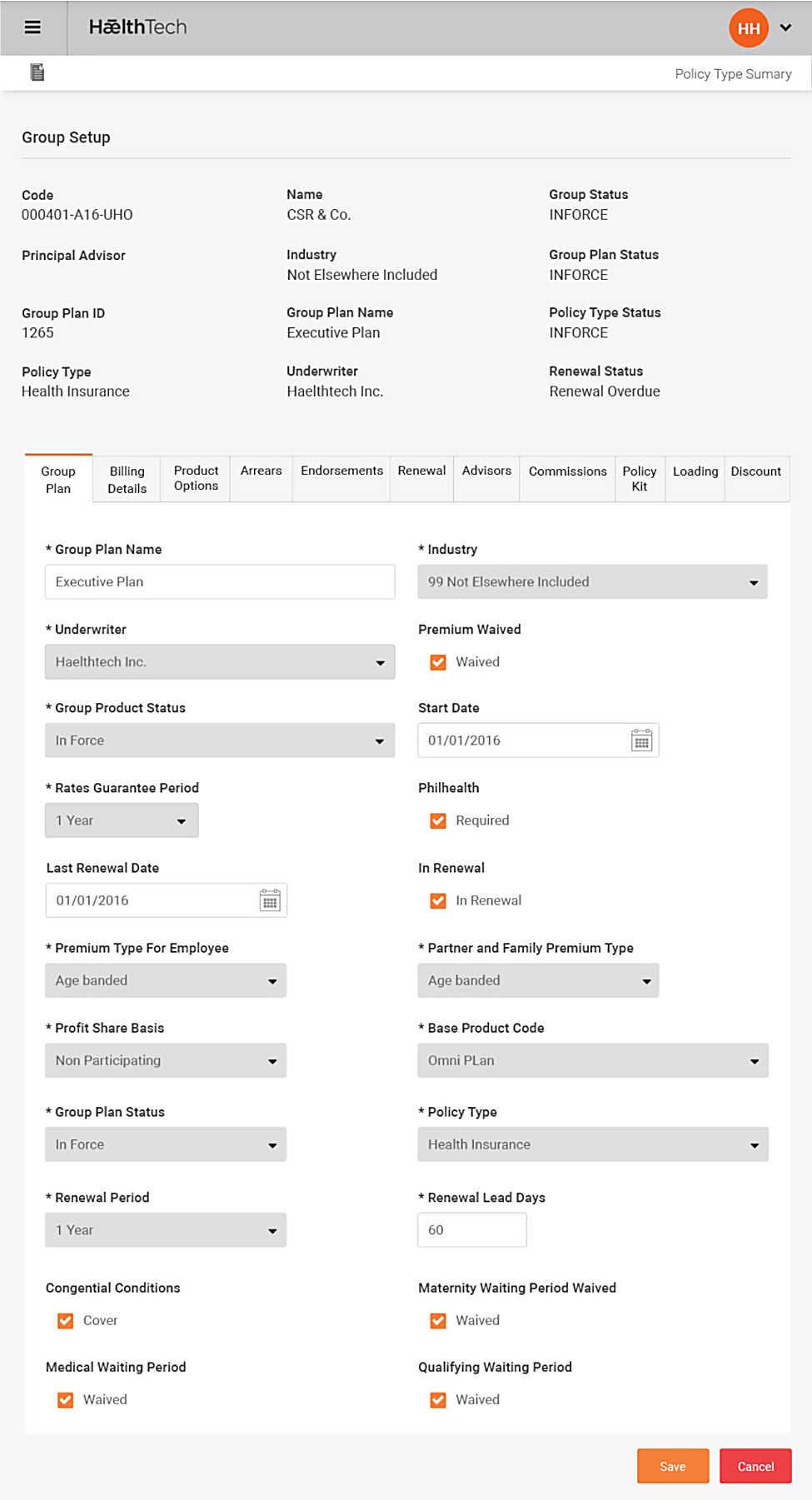
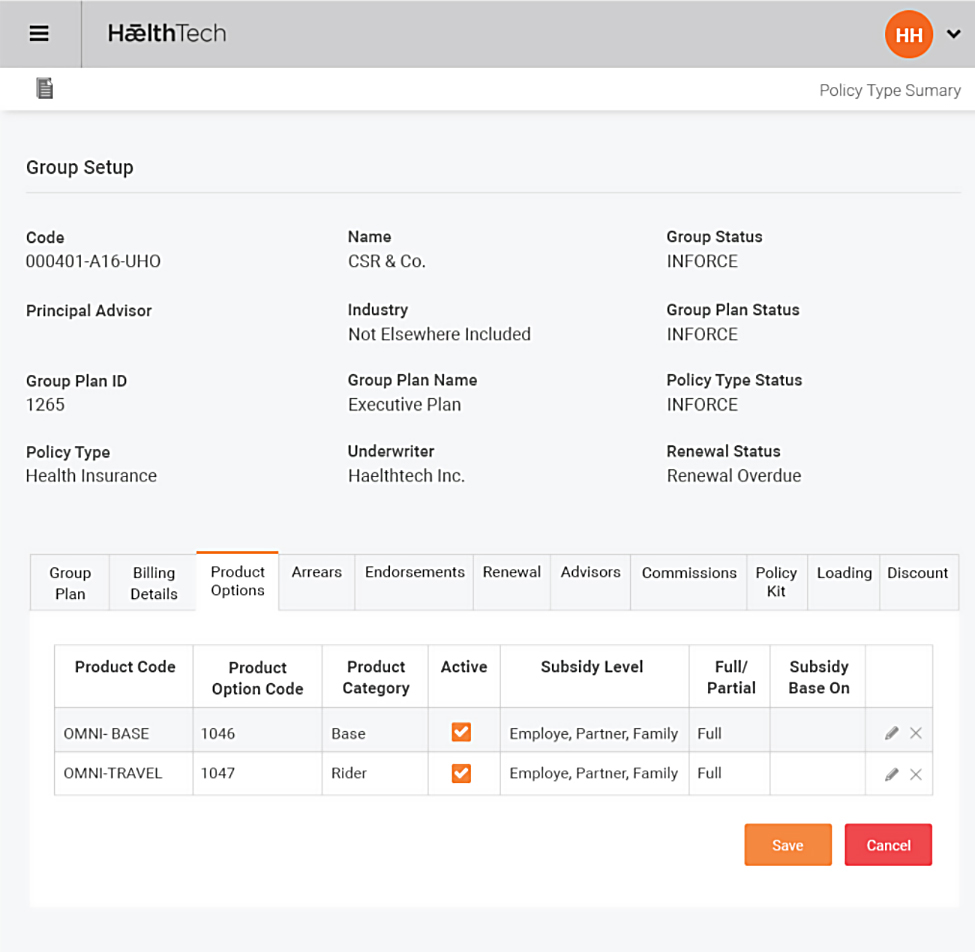
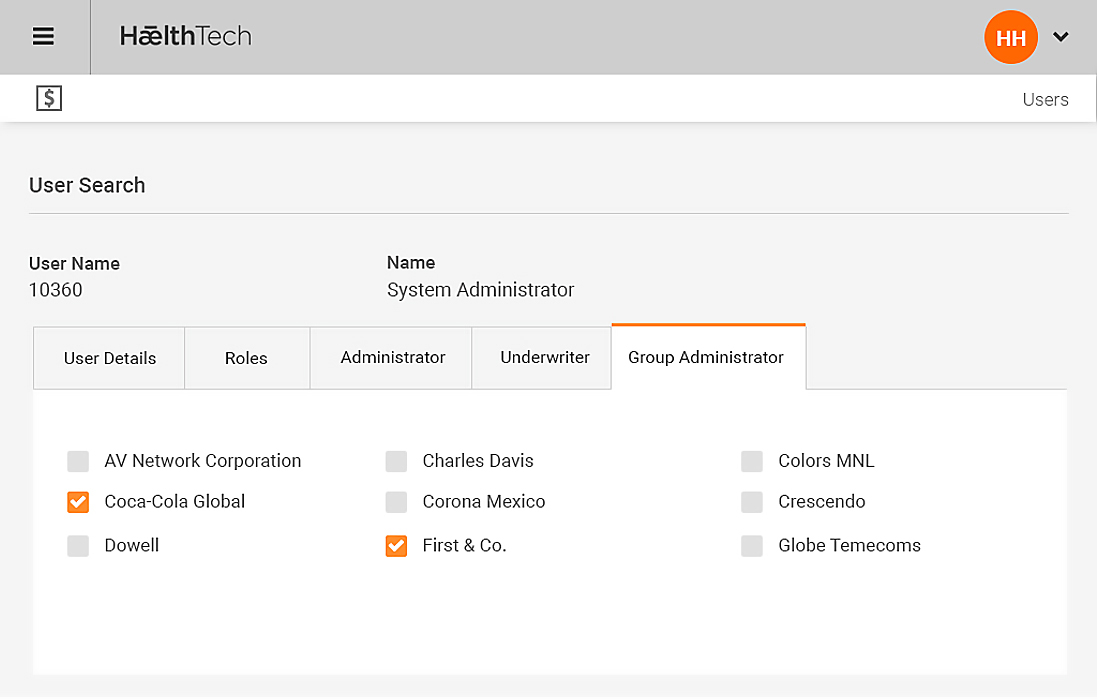
Figure 14 - The Omni Back End Group Plan
A full range of self-managed options are available to the member including:
- Name and Address
- Bank account details for payments and claim re-imbursements
- Schedule of benefits
- Form download
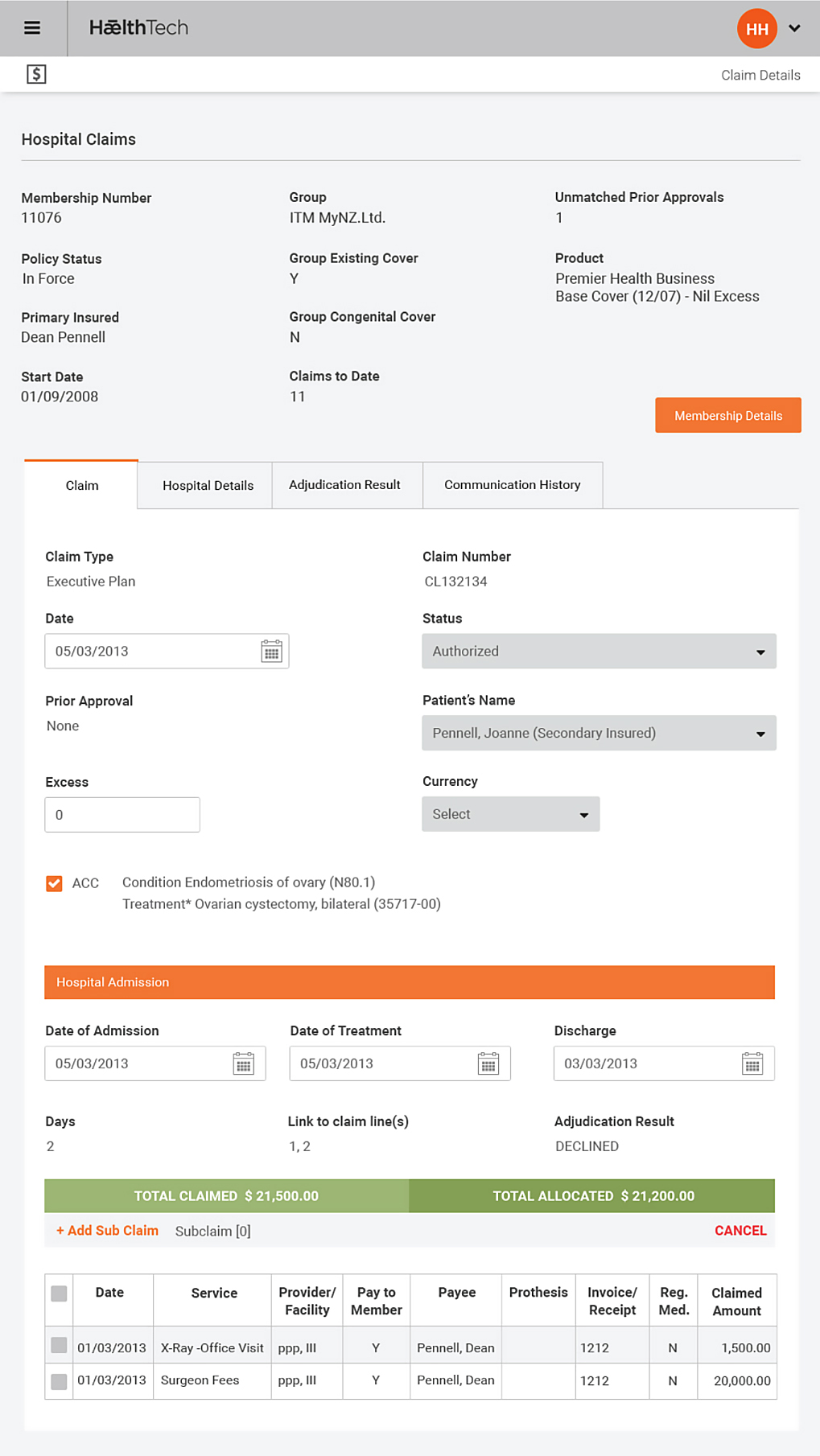
Claim Entry
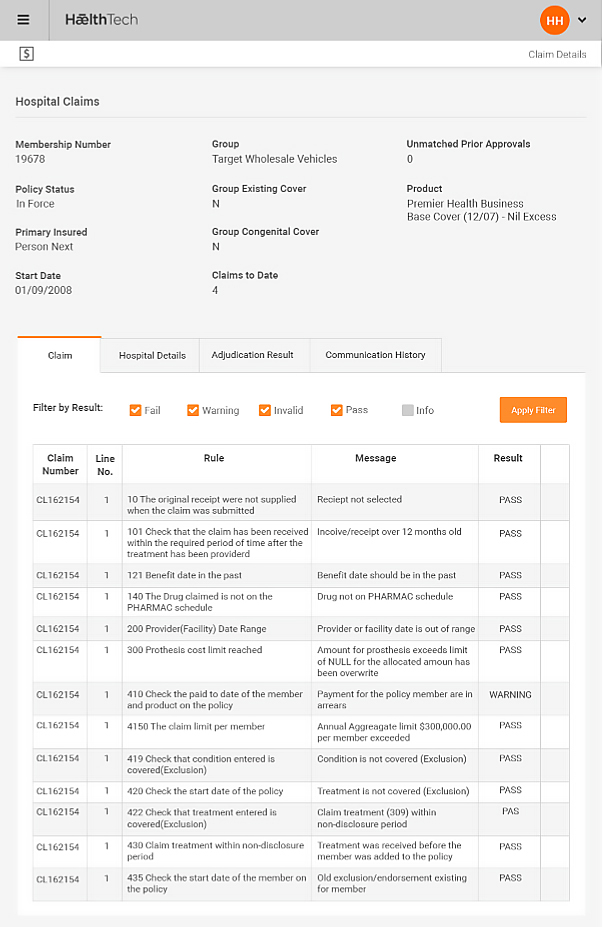
The Omni Benefit Plus system allows members to enter claims for reimbursement. Once entered, the claim is passed to Omni administration staff to be processed under the strict rules and adjudication controls supported. These adjudication rules can be configured to your requirements.
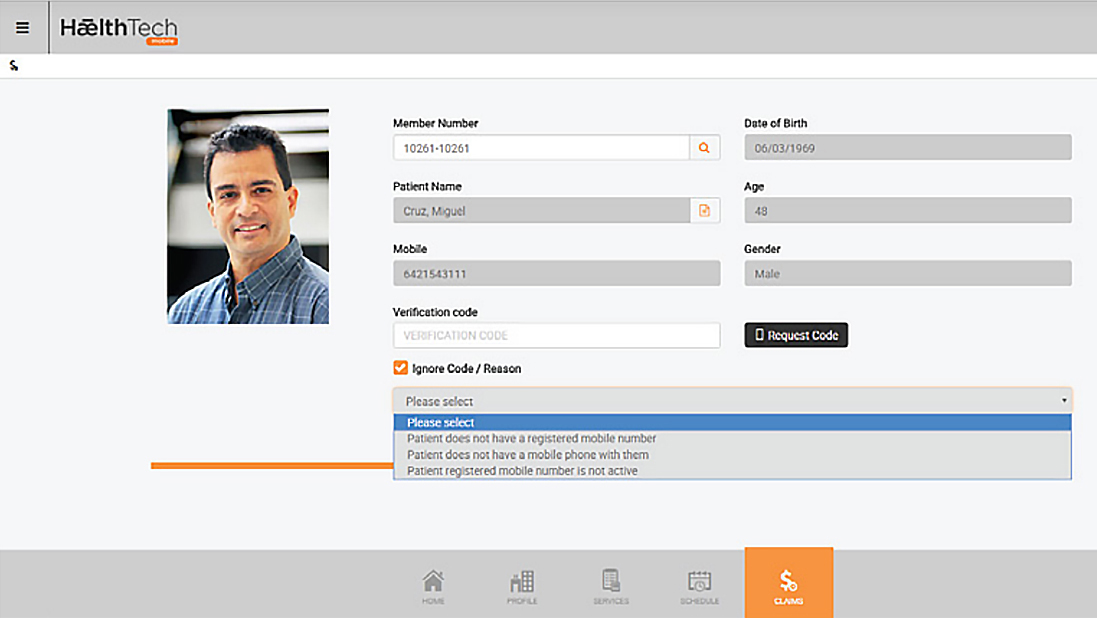
Figure 15 - Claim Entry
Members can view claim progress as well as product cover options prior to claim entry.
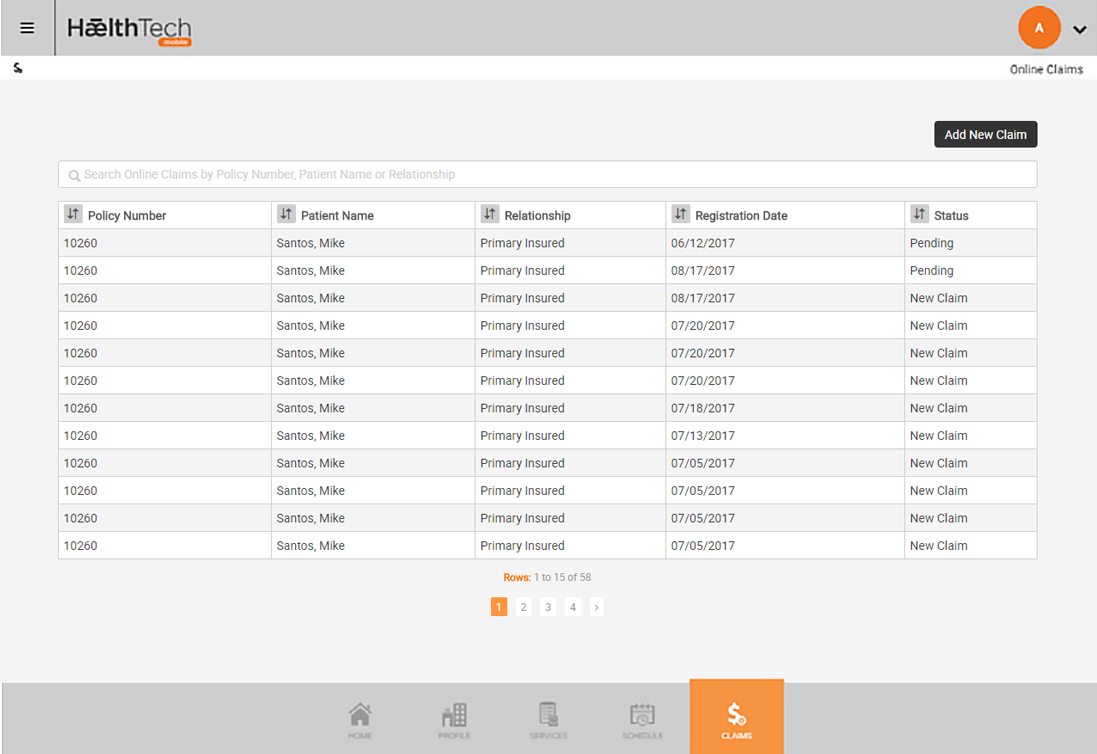
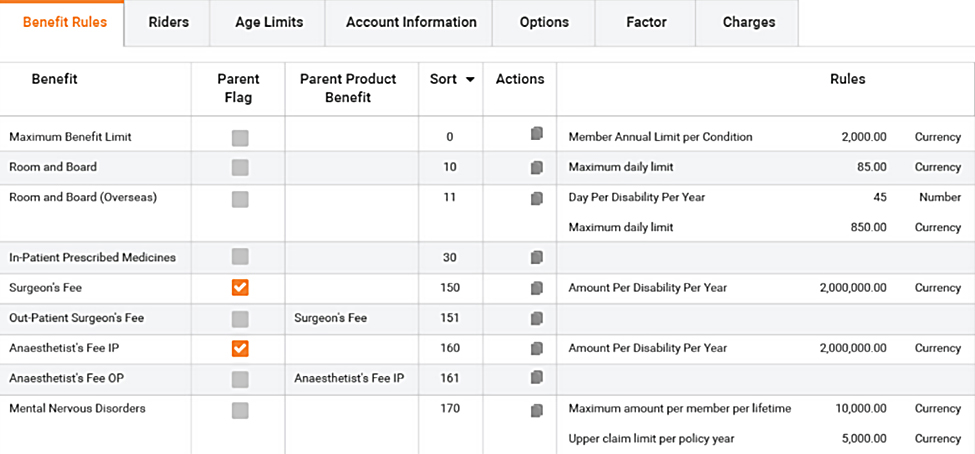
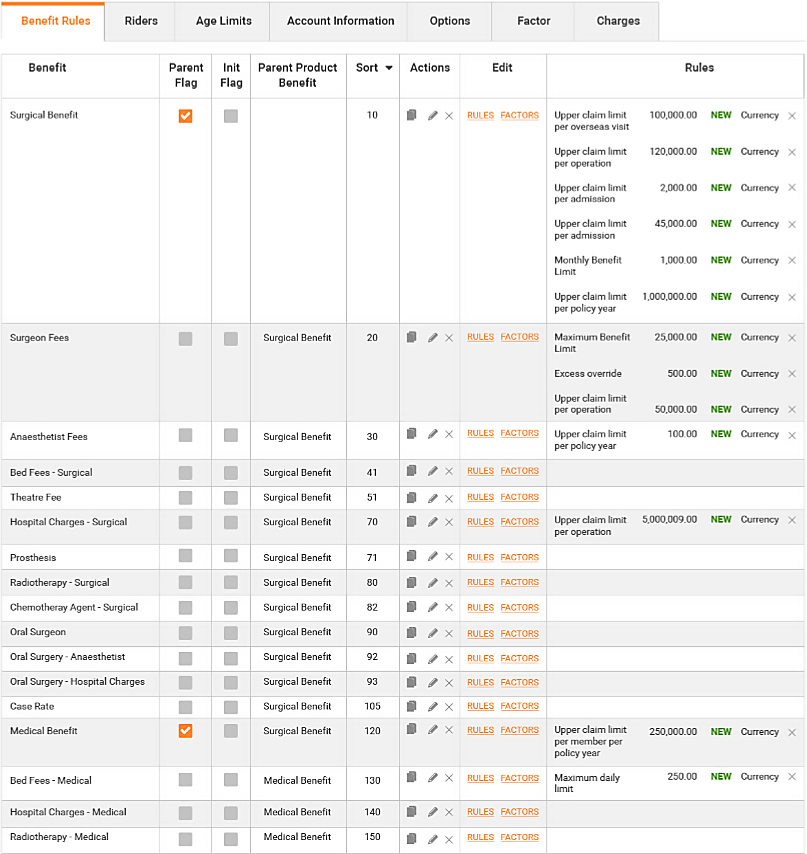
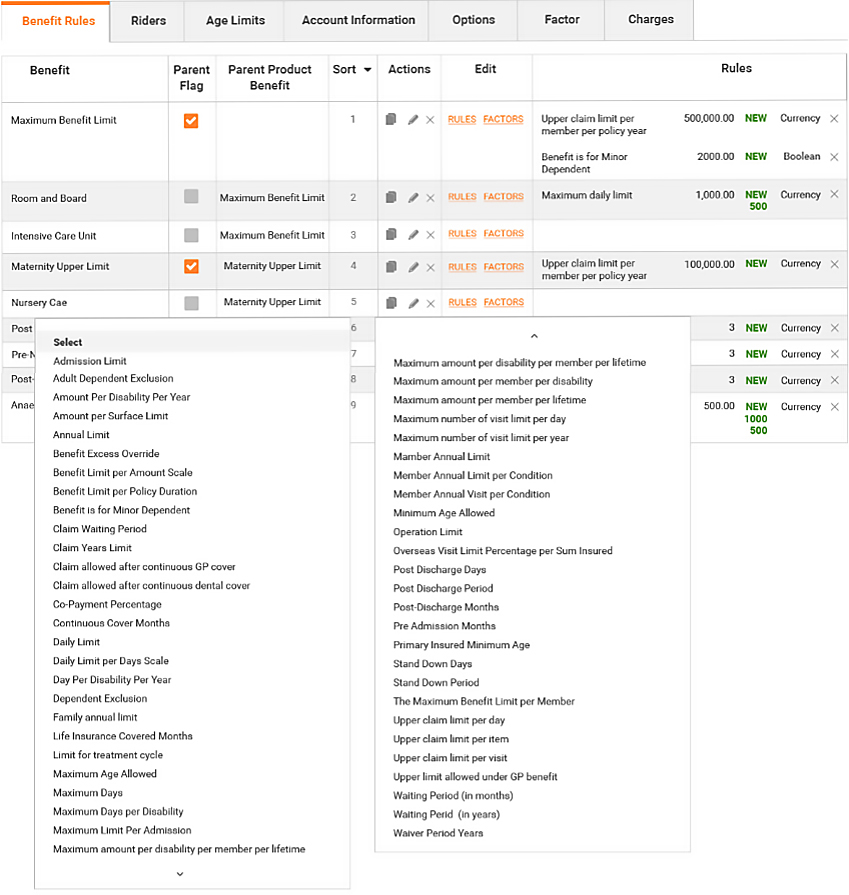
Figure 16 - Sample Rules List available from a drop down list to apply to an established benefit
This allows members to see rapid completion of the claims and payment process. This is achieved by allowing the direct input of a large volume of claims into the system by members, and real-time analysis of claims, fraud detection and controls under the claim adjudication engine rules, and loss ratio management control.
The coupling of the Omni Benefit Plus front end to the Omni administration engine is a unique construct allowing overall, superior risk management.
Dashboard
Omni provides a range of reporting options - from customary back end reports to dashboard views of relevant data.

Member Lifestyle
Members lifestyle options and information form a complementary addition to health insurance.