About HǣlthTech
Reduce risk, spend less, more efficient Employee Benefits Admin
HǣlthTech is an advanced software company specialising in highly cost effective, flexible, web and mobile based health insurance and risk management systems for fully insured groups and groups that self insure.
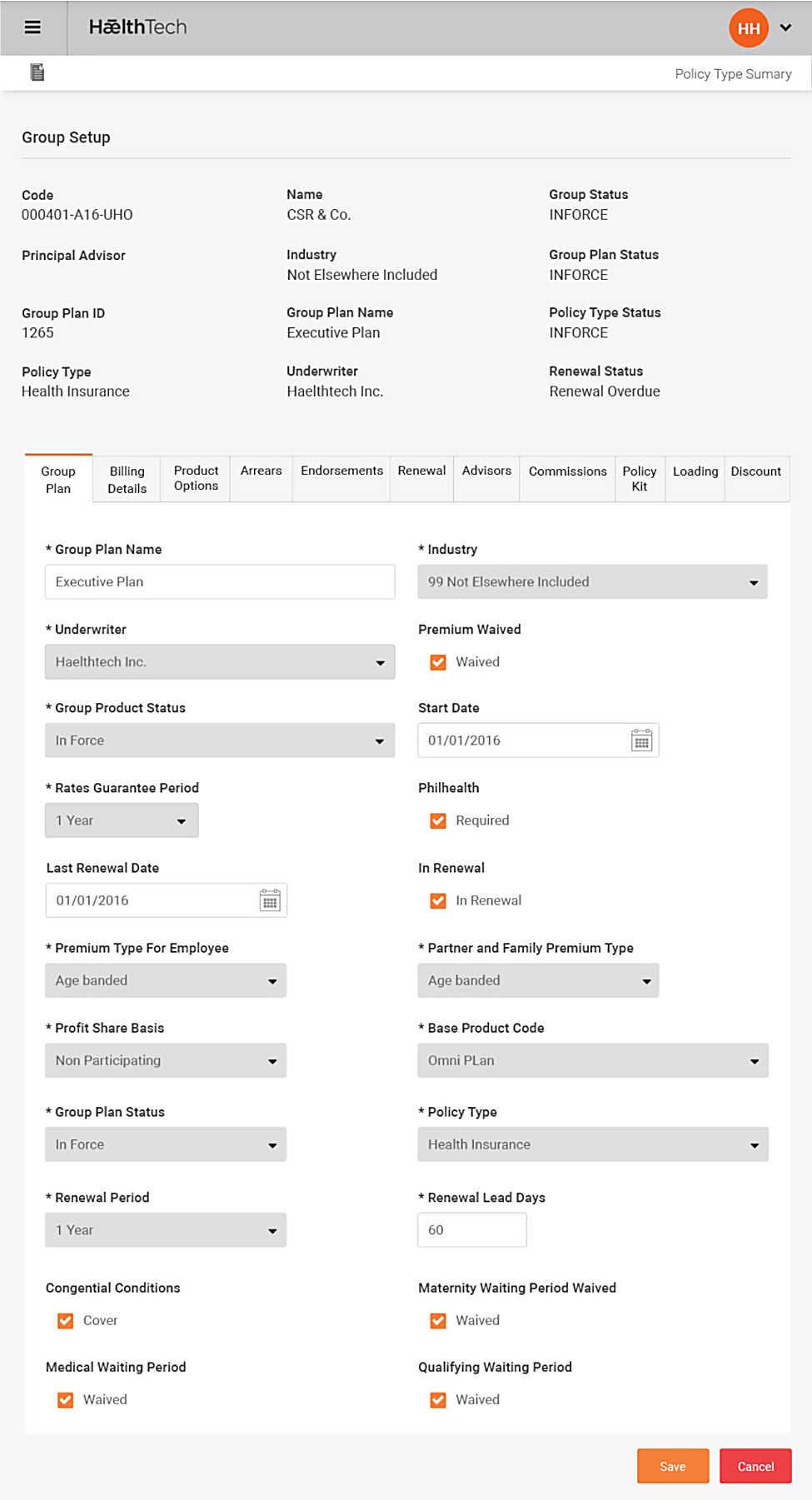
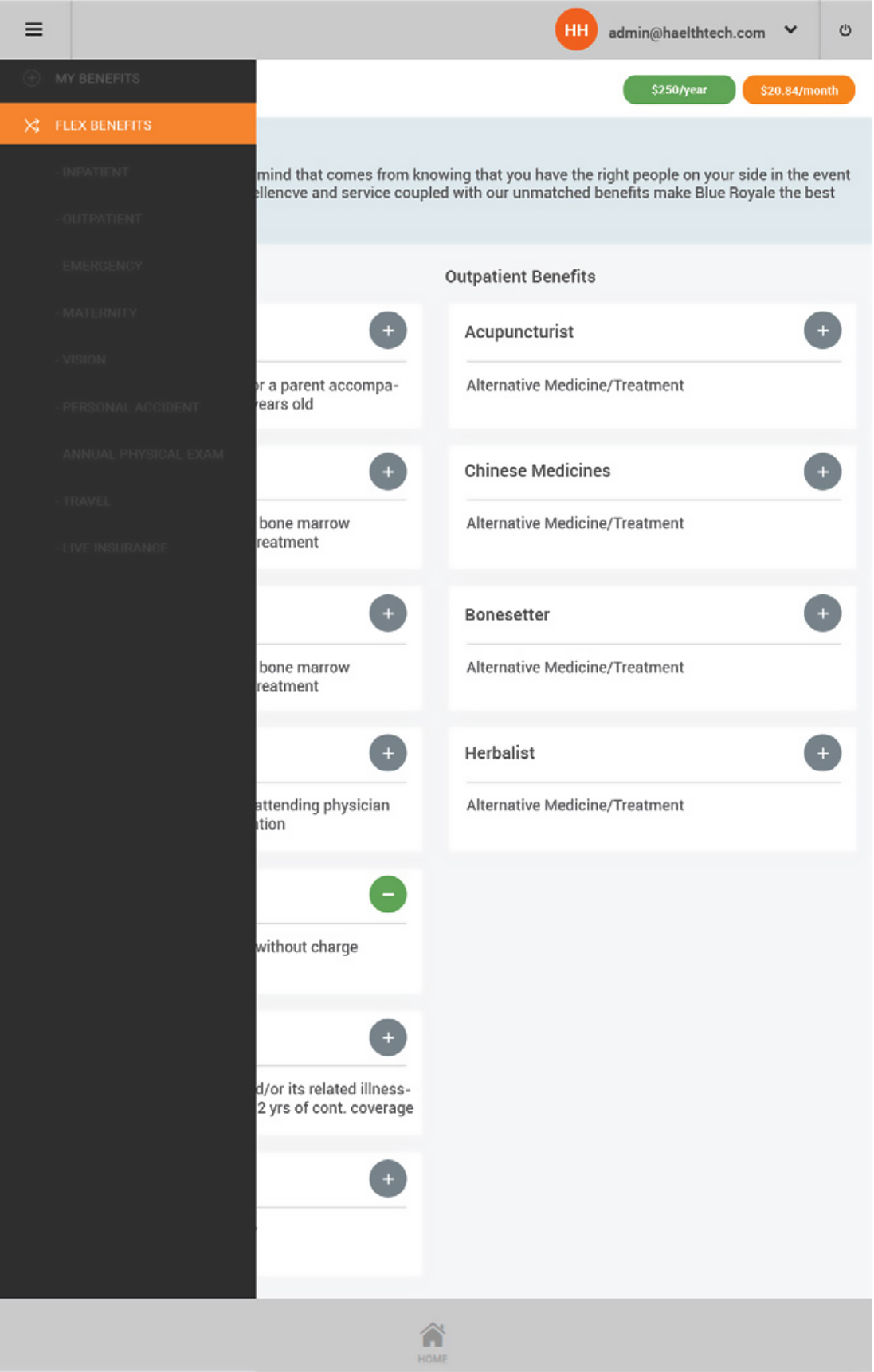
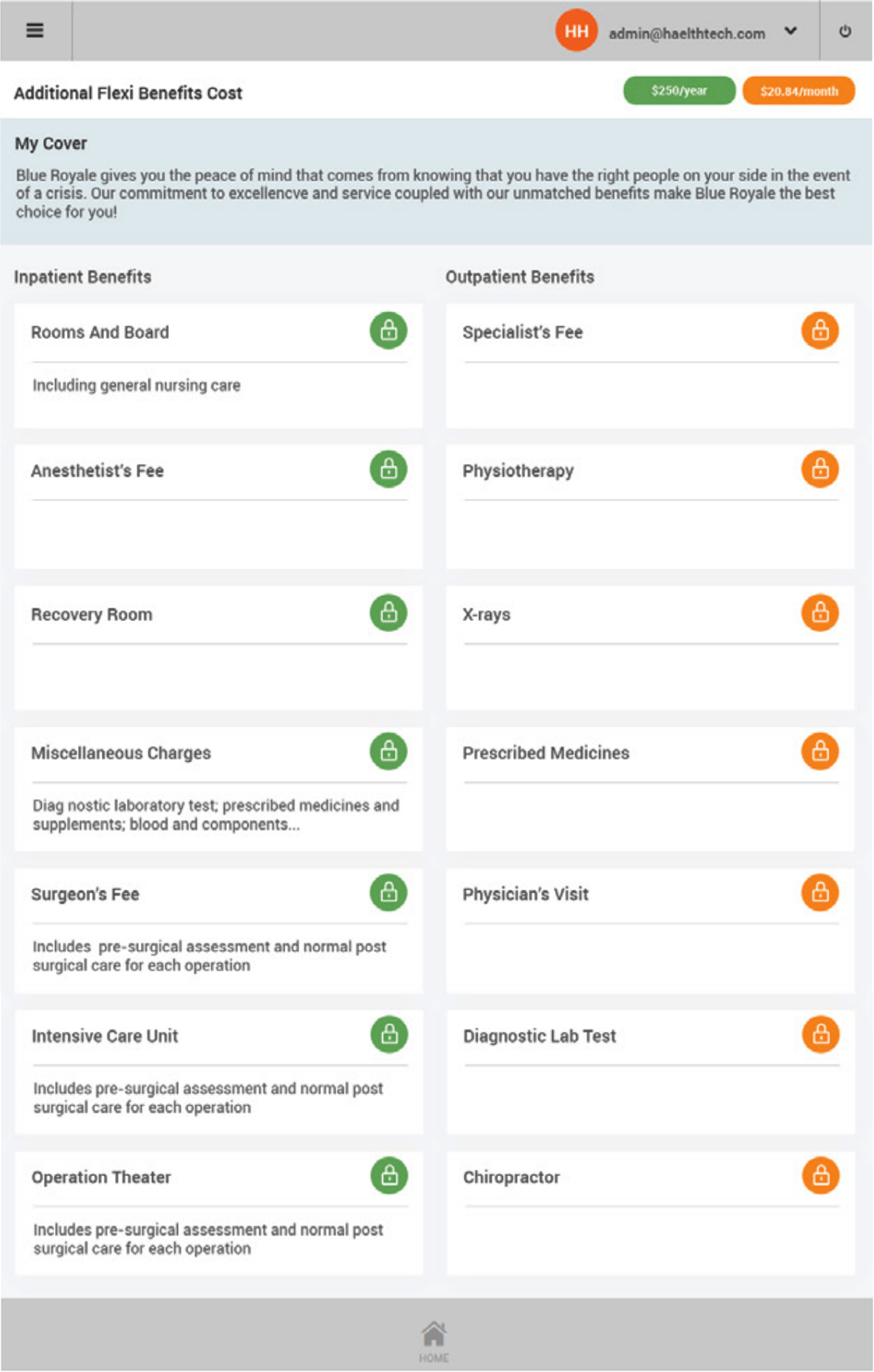
Omni is fully integrated to support every step in the health insurance value chain is based on mobile self-service to share the information and workload with underwriters, groups and members.
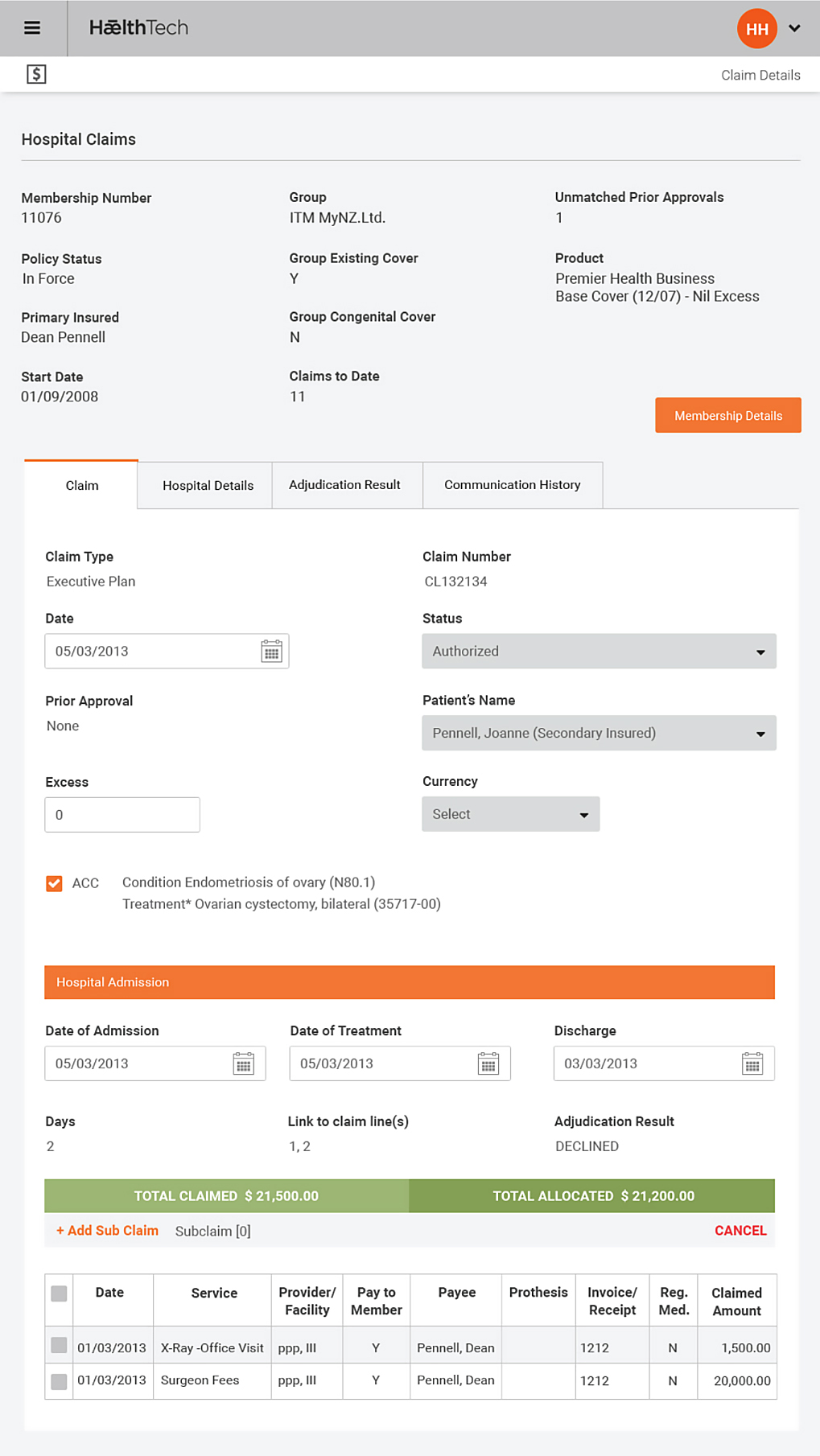
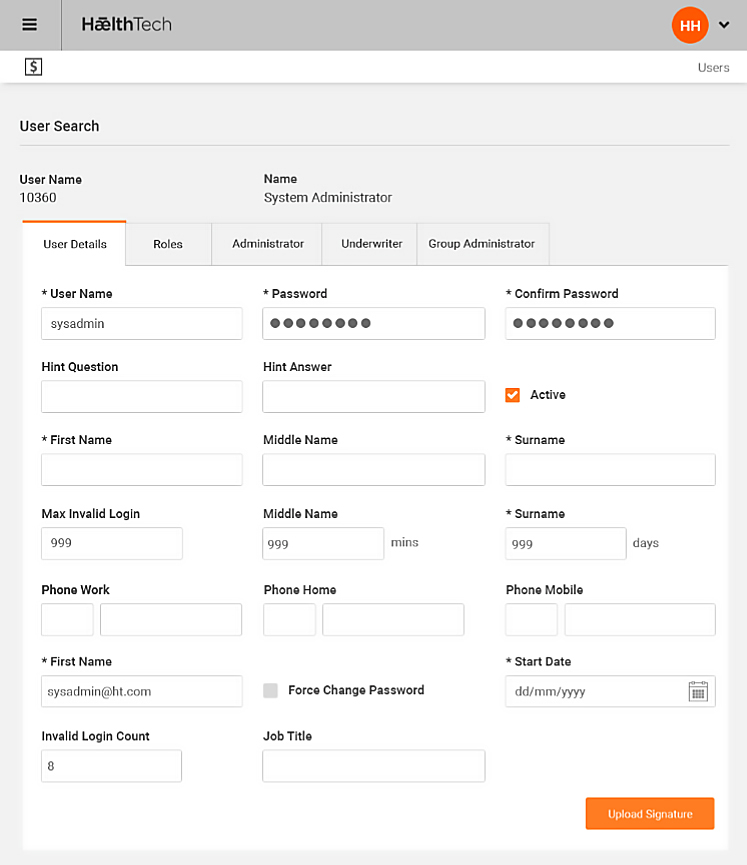
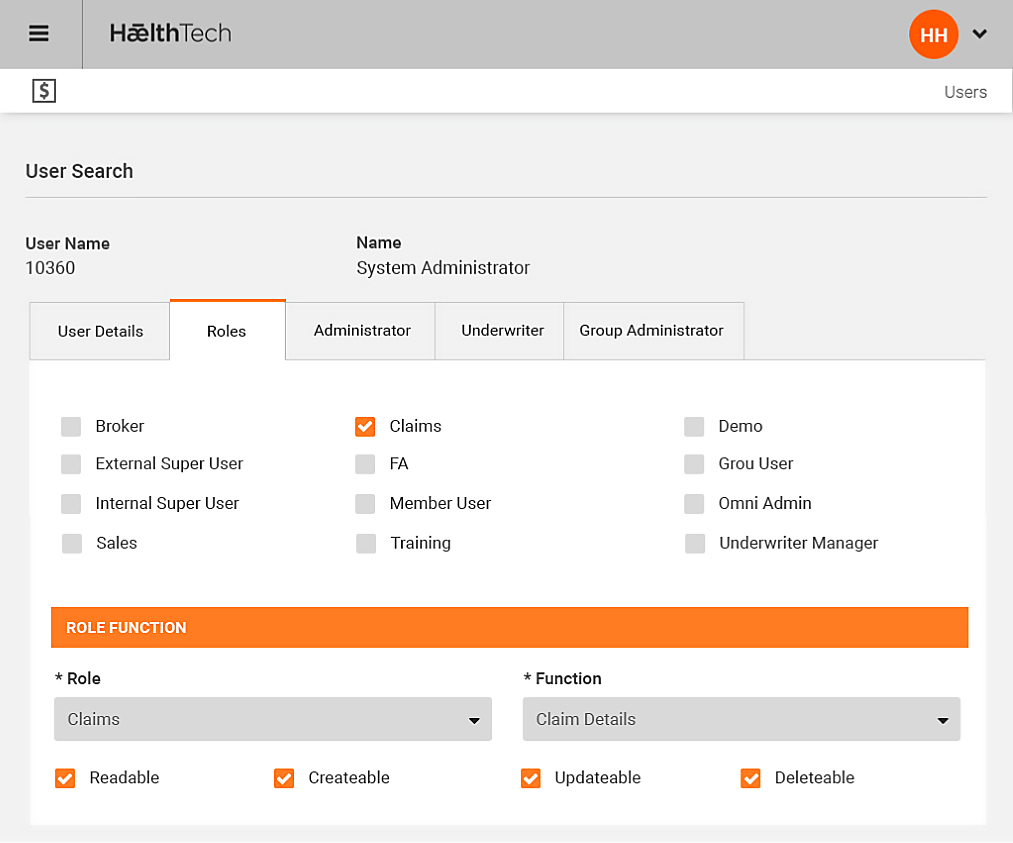
Its straight through processing environment enables administrators to concentrate on claims and case management instead of routine administration activities as external parties can update and maintain their own information.
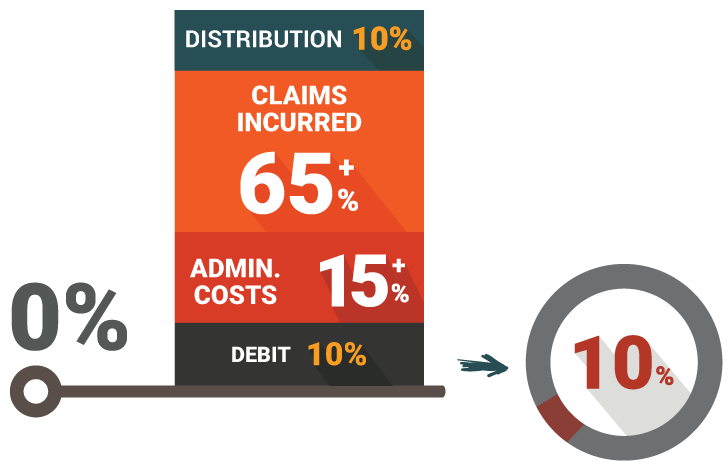
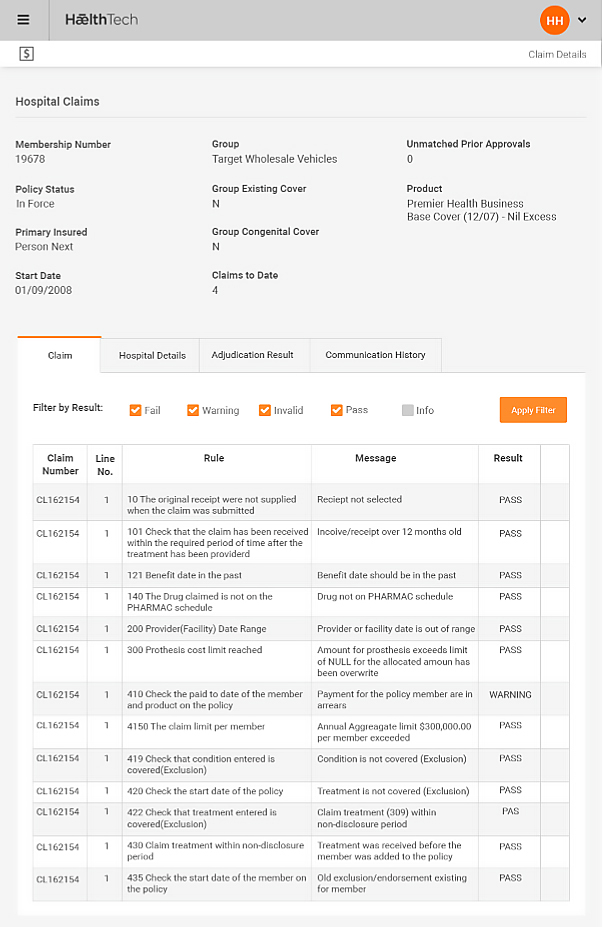
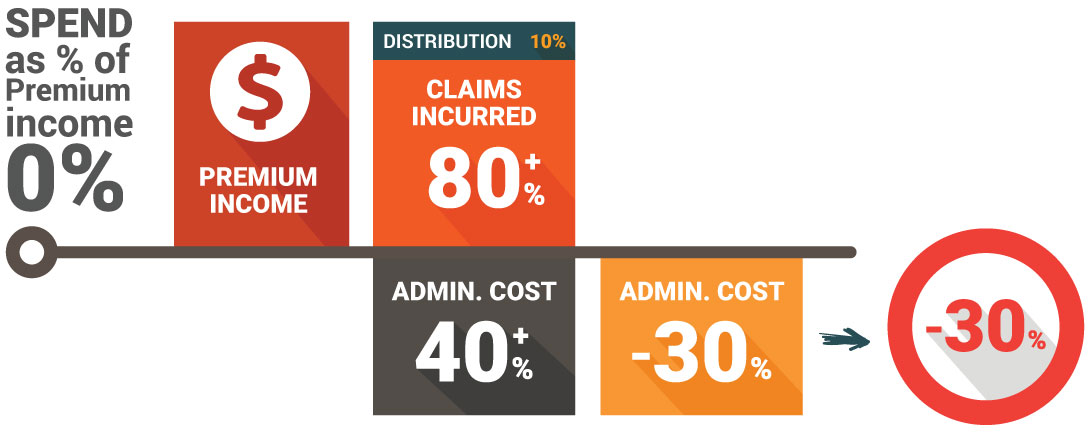
By dramatically reducing administration costs and ensuring that claims are swiftly and objectively processed, insurers can manage risk and keep loss ratios at optimum levels.
Omni has been designed using the combined expertise of our senior executives and technical team, utilising their many years knowledge from working in the international health insurance sector.
OMNI is based on open source technology that utilises standard architectures and frameworks based on Java Enterprise Edition platform (JEE).
OMNI application uses a multi-layered distribution application model, which means that the application logic is divided into component layers according to functionality. The various application components are isolated into their specific container installed on different machines depending on which layer the component belong.
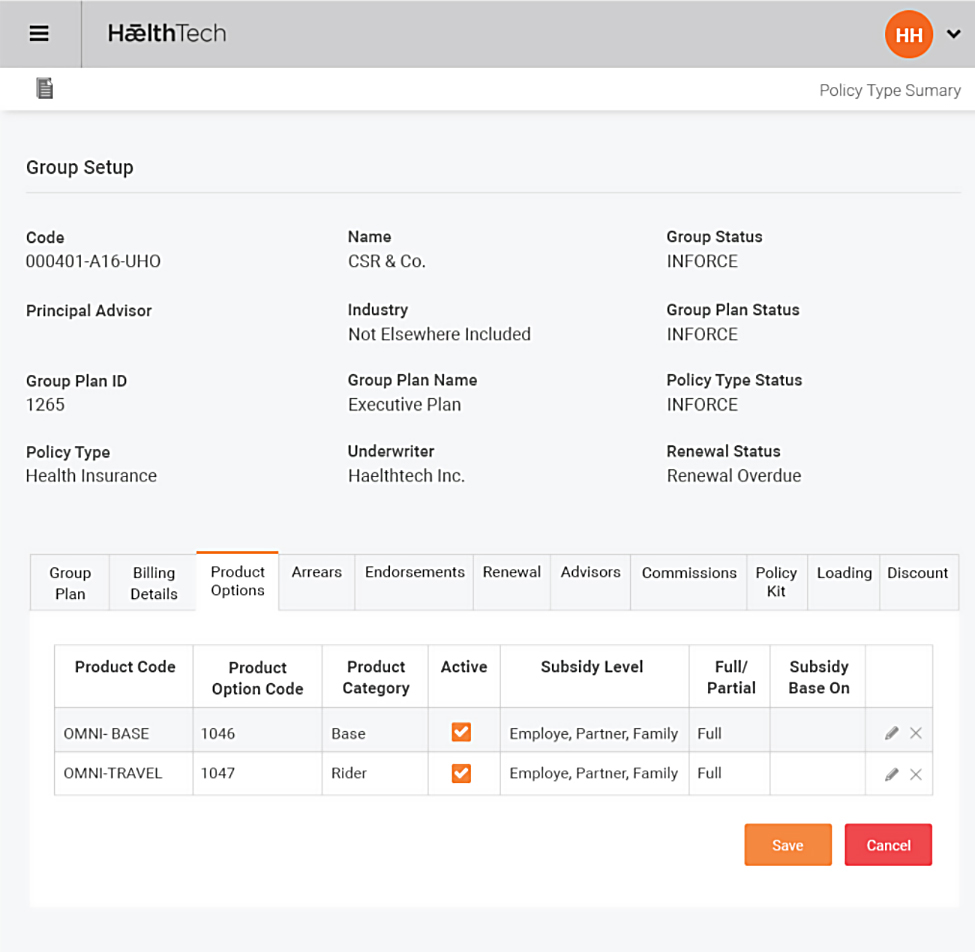
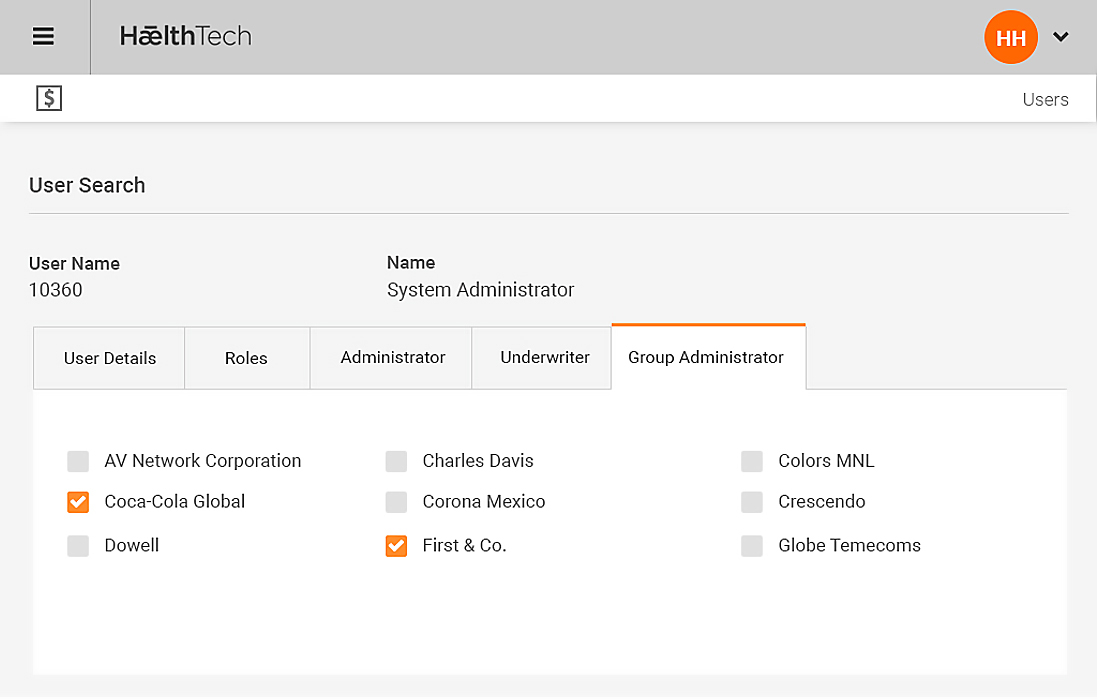
Omni is a fully integrated, multi-tenant solution built around core business information such as Groups, plan definitions, policies and related products and product bundles.
Omni Data Platform is fundamentally versatile, providing linear, scalable storage and computing across a wide range of access methods from batch and interactive to real time, search and streaming. Each Omni instance is capable of handling unlimited underwriters, thereby ensuring information can be obtained easily via management reporting tools. This allows centralised integration with external Underwriter or Group systems as required.


Working as One
Our web and mobile solution is collaborative, integrated and accessible by all the users of health insurance so they can work as one, including:
- brokers, insurers, members and groups
- third party administrators (TPAs) in the group insurance business
- large insurers offering their own group insurance products
- insurance brokers organizations
- large organizations providing self insurance

The Challenges
- Most insurers continue to offer health insurance at an overall loss to protect high profit lines e.g. Life policies. Many insurers are running health portfolios with loss ratios greater than 100%
- Premiums are increasing at over 10-20% per annum to cover increasing health costs, making premium renewals more difficult to justify to the insurers customers
- Products are becoming more and more generic by carrier with little point of differentiation, creating primarily price-based competition
- Administration costs are factoring as a high percentage of premium
- Claim loss ratios are out of control
- Provider "over-servicing" and “over utilisation” of cover causing dramatic increase in claims payments
- As provider-sided health insurance management is difficult, many insurers outsource risk-based functions to Third Party Administrators (TPAs) which eliminates effective risk management and control from the insurer
What the Marketing Seeing
Best Practice