Claims Processing
Solutions
The Problem
Insurers cannot deliver a profitable Group Health business and yet carry all the risk.
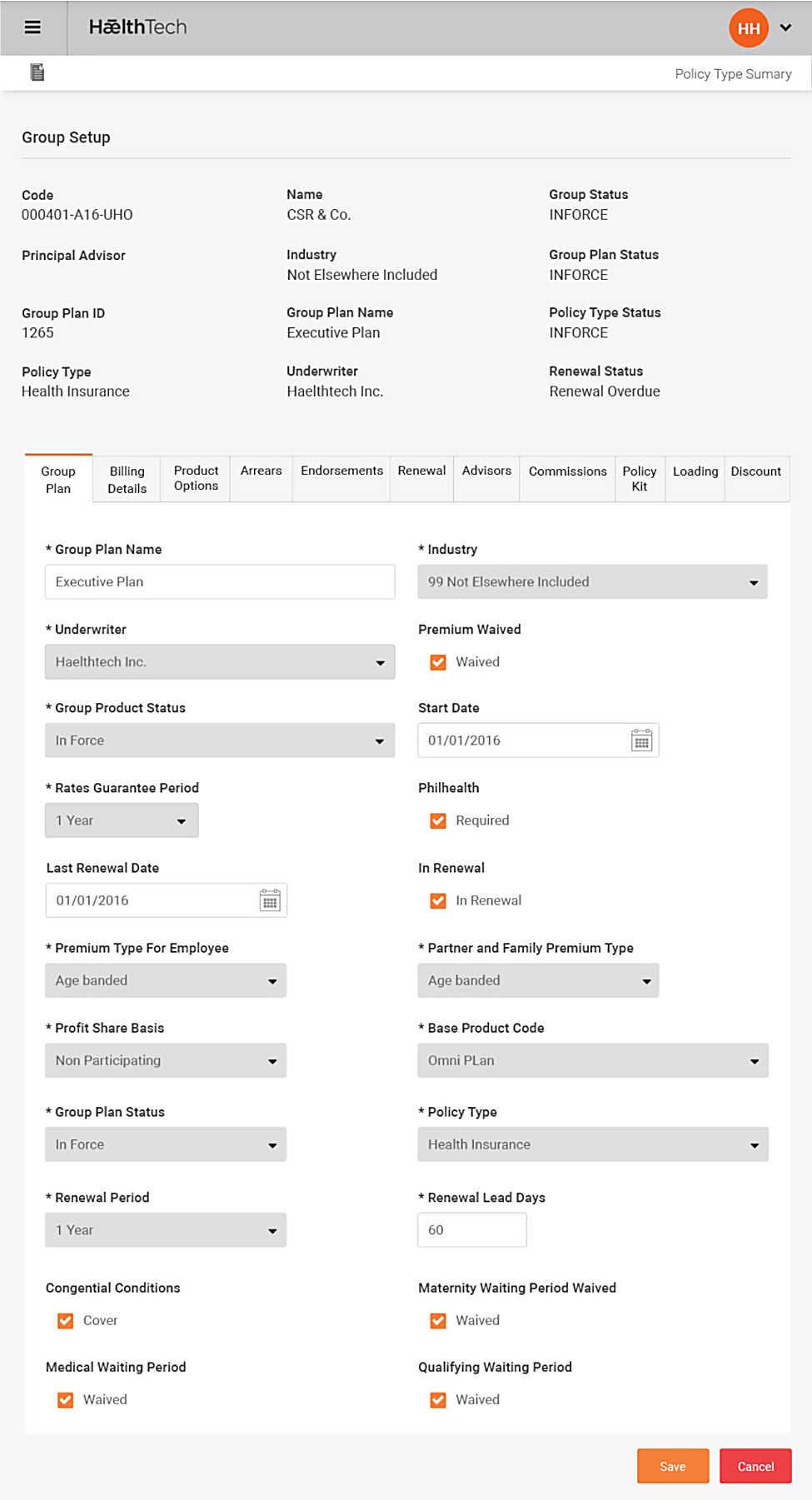
HǣlthTech workflow engine covers processes such as policyholders on-boarding, claims filing, management, adjustments, pre-authorisation, customer notifications, payments and many more.
- Over-payment of claims vs. underwriting rules
- Member identity fraud
- Claims inflation at provider level
- Member identity fraud
Excessive cost around member and policy administration
- Claims not properly adjudicated from point of treatment, largely manual processes
Wholesale inefficiencies throughout the value-chain, adds high cost
- Members (inc. HR) -> Provider -> Agent -> Insurer
- Most insurers continue to offer health insurance at an overall loss to protect high profit lines e.g. Life Insurance
- Premiums are increasing at over 20% per annum to cover increasing health and administration costs
- Administration costs are factoring as a high % of premium – usually > 30% - especially with TPA’s
- Products are becoming generic by insurer driving price rather than value based competition
- Provider “over-servicing” and over utilisation of cover causing dramatic increases in claims costs
- Outsourcing to TPA’s eliminates effective risk management and control from the insurer
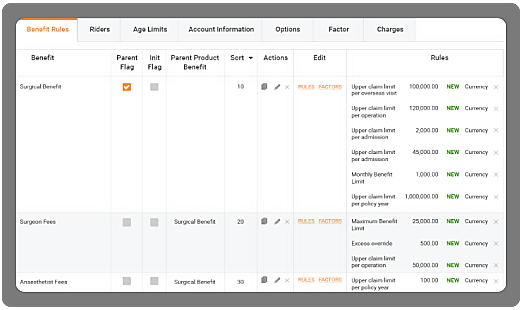
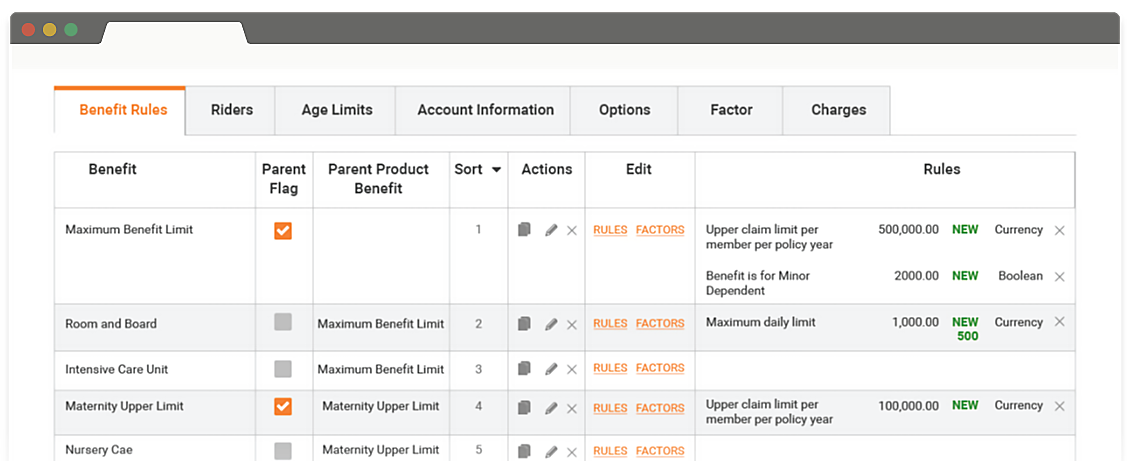
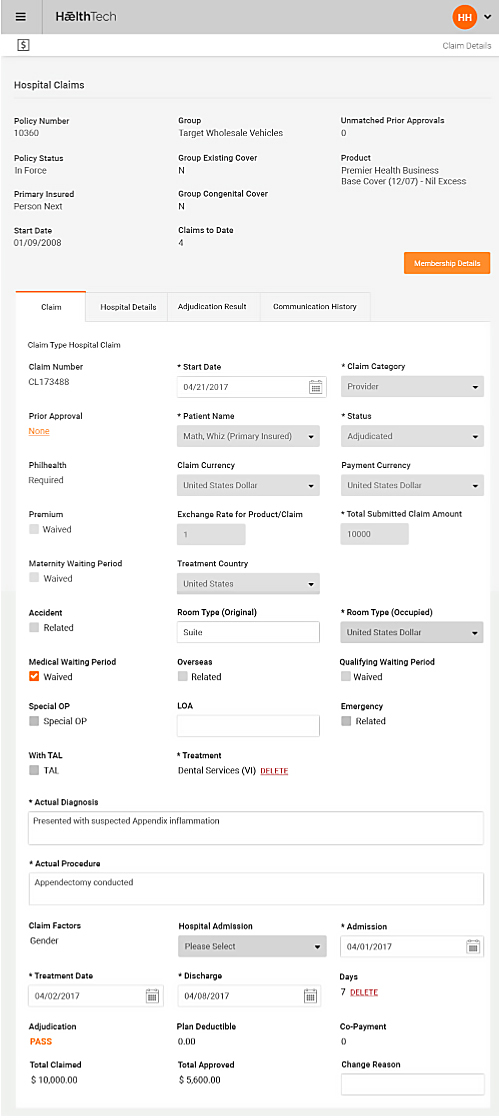
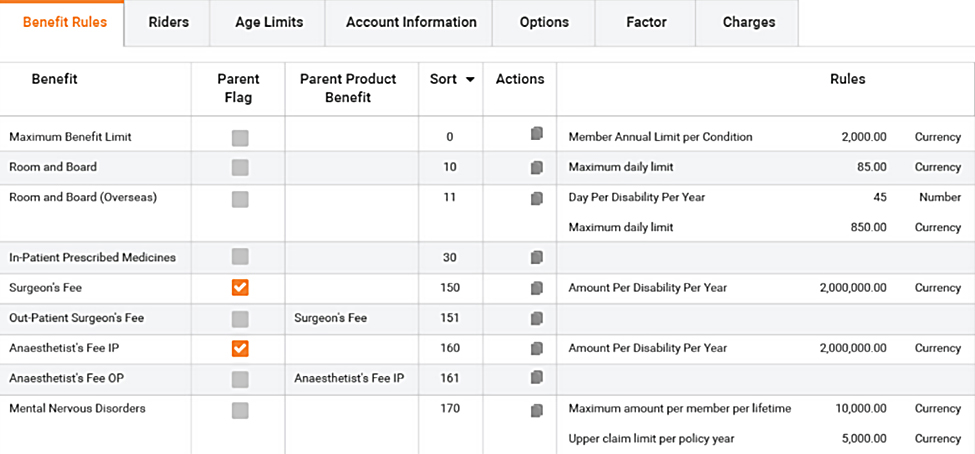
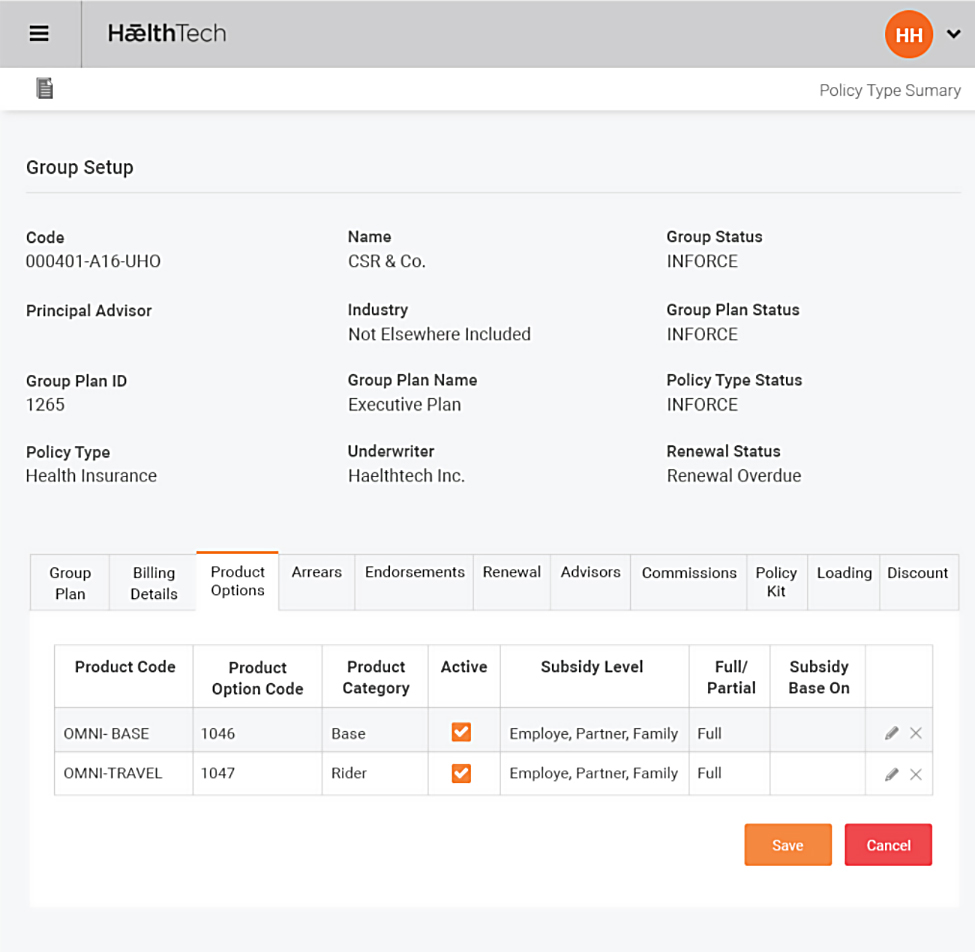
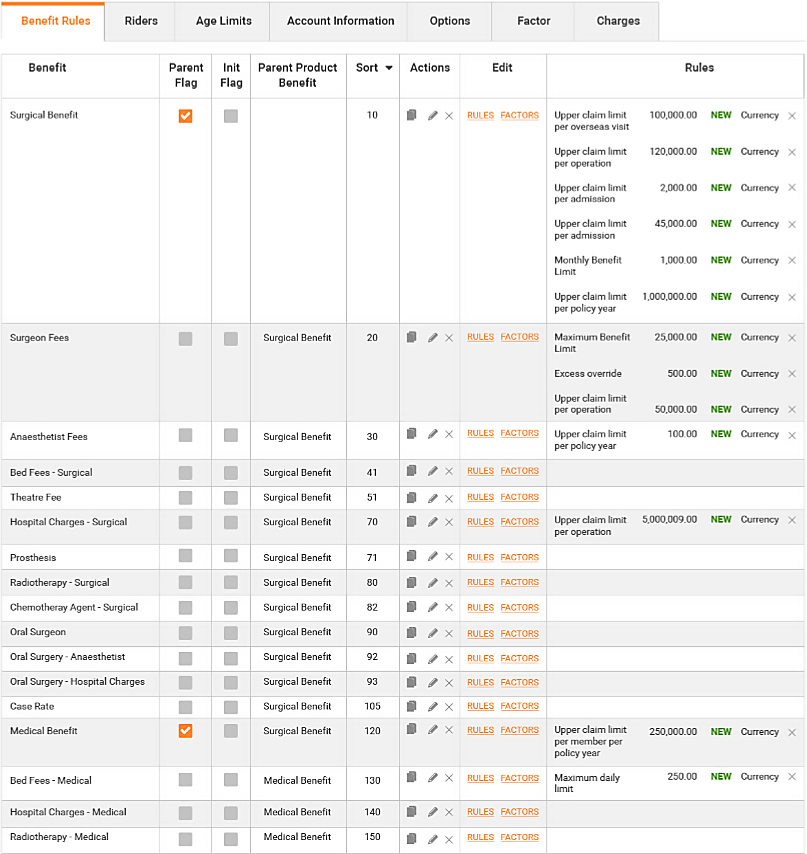
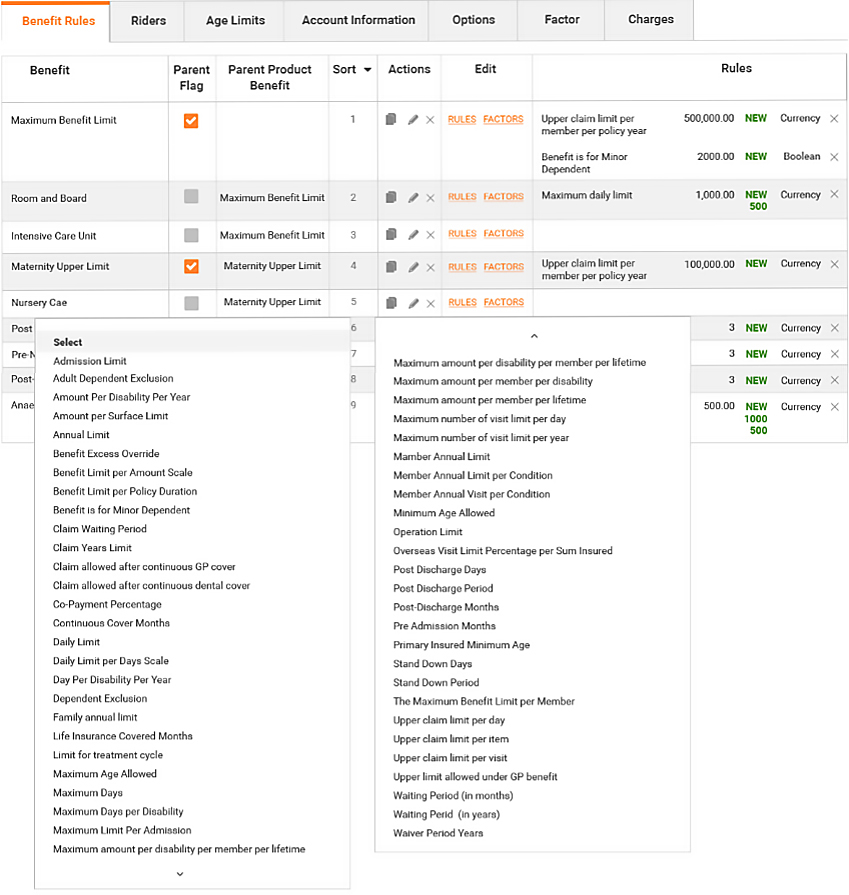
- Omni embeds the underwriting and policy rules into the claims adjudication engine for immediate use at claim time
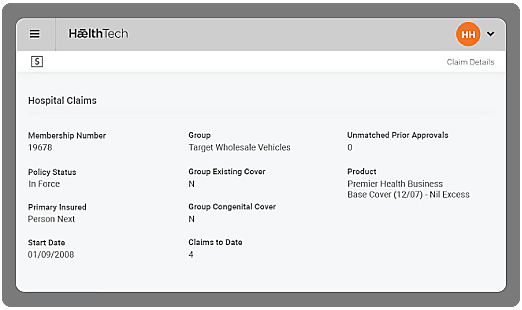
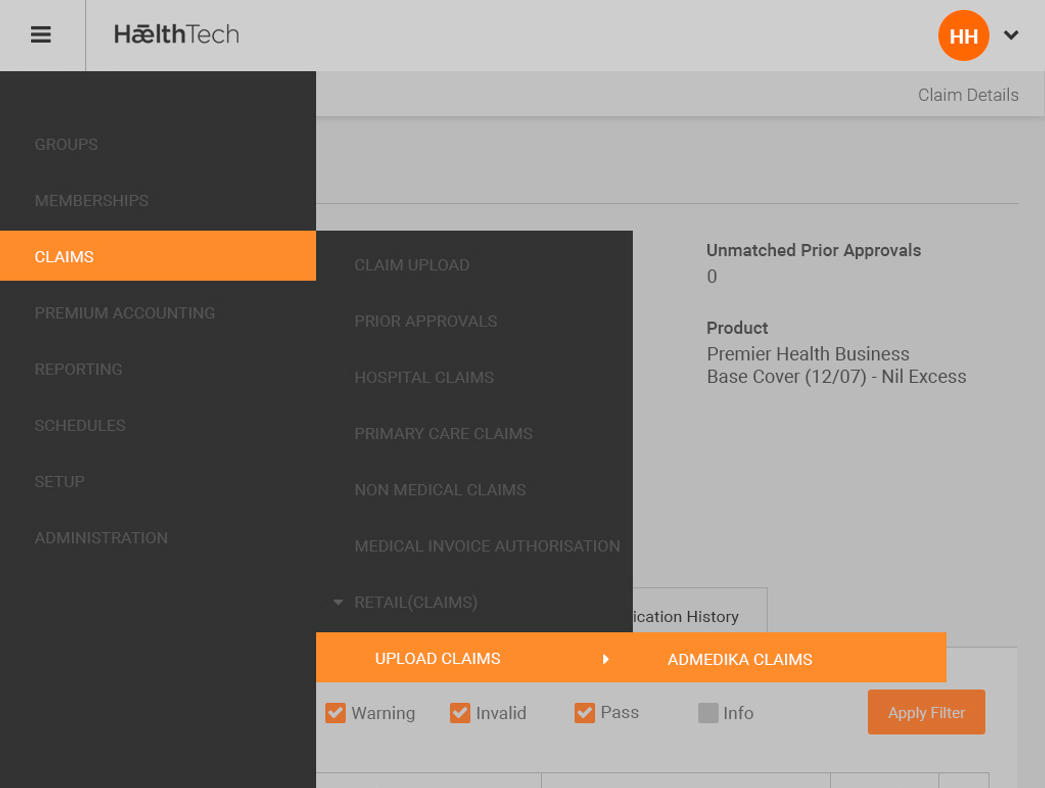
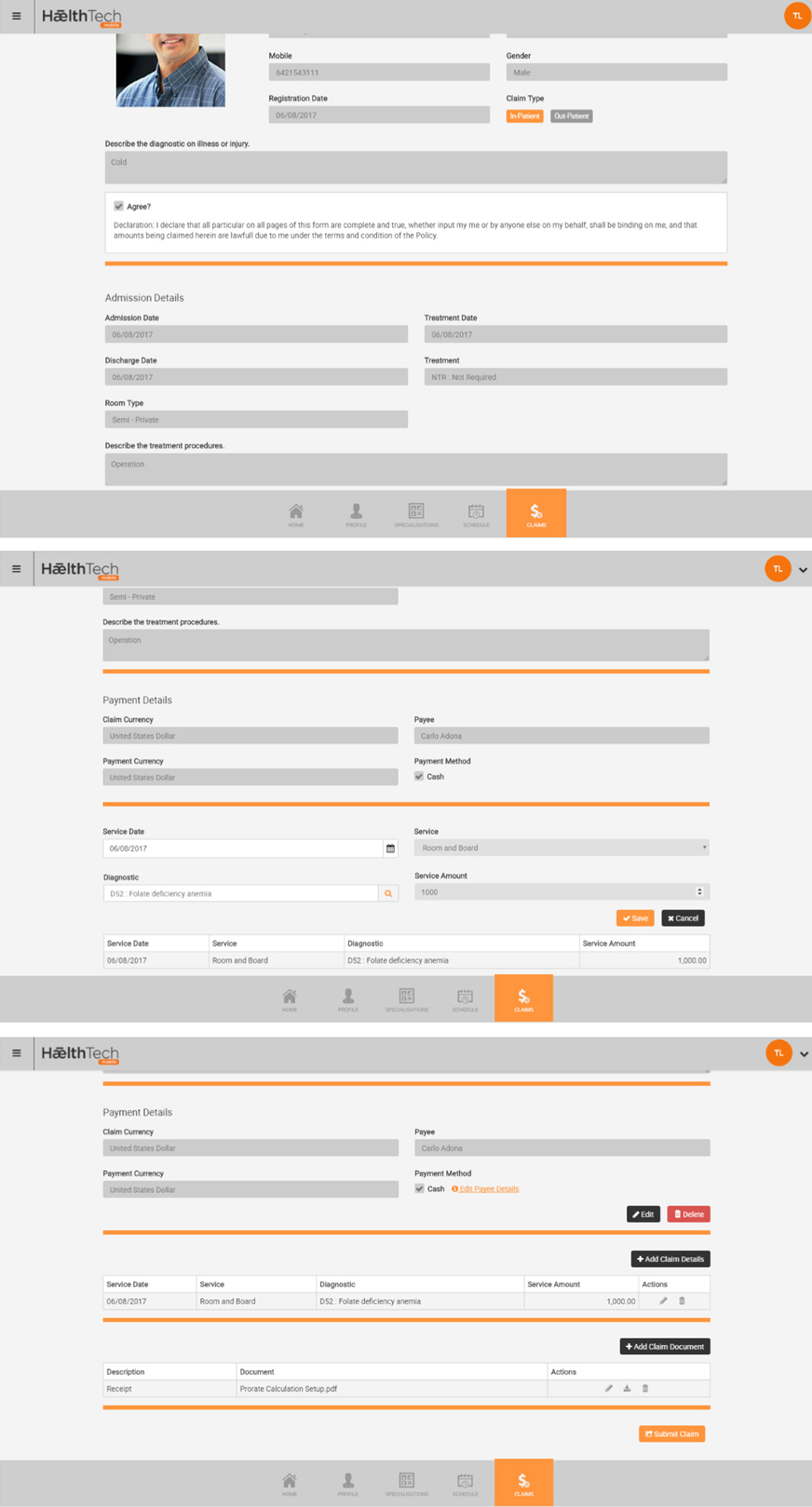
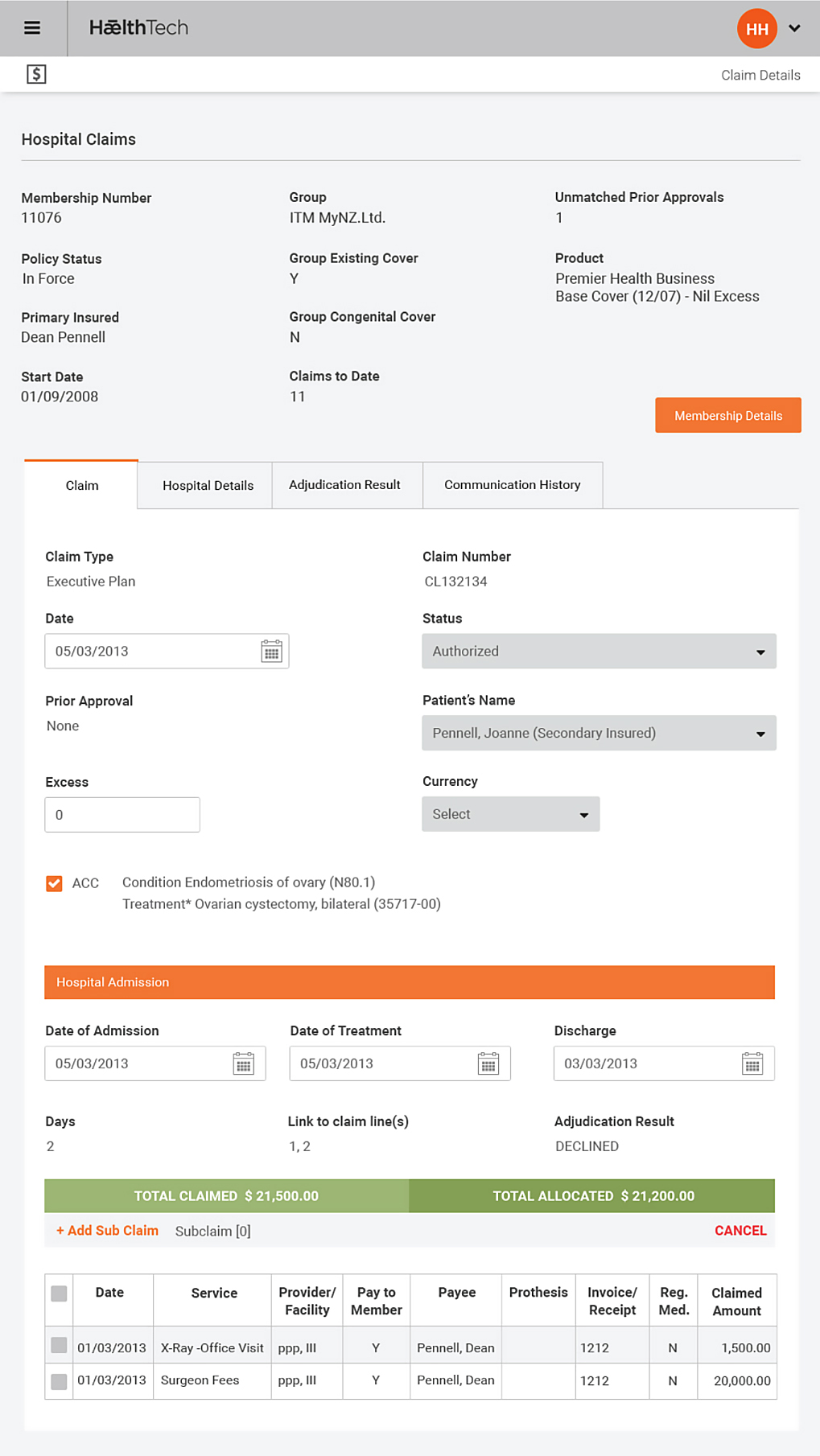
- Omni manages the process from pre-approval to claim payment in a single workflow without re-entry of data
- Omni Auto-adjudicates >95% of claims
- Omni Utilises API driven interfaces to talk to other systems e.g. Hospital Management Systems
- Omni Mobility allows for member / provider / group HR entry removing heavy claims admin overheads
- Omni captures all elements of claim risk at admission and reduces latent exposure to over utilised benefits and non-payable charges
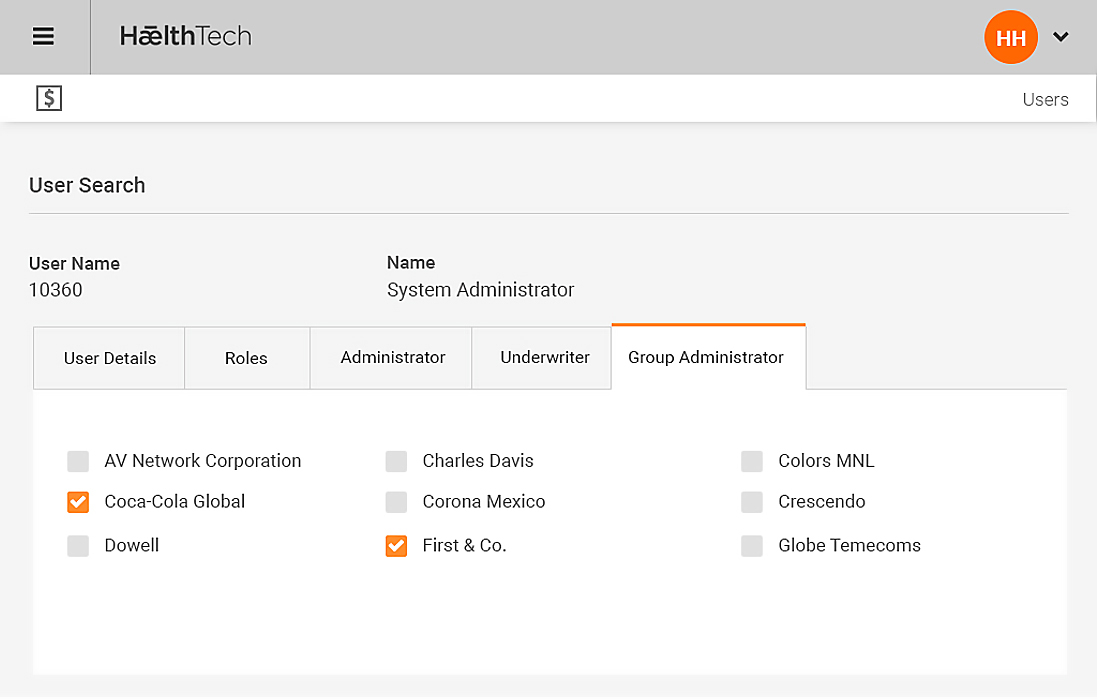
- Omni allows opex based administration functions to be outsourced to the TPA
- Omni allows the insurer to give TPA access to the automation & complexities of the claim system via the internet or mobililty
- Omni allows the Insurer to manage risk in real-time
- Omni ensures that transactions are real-time and data is not mismanaged as it is passed from point to point
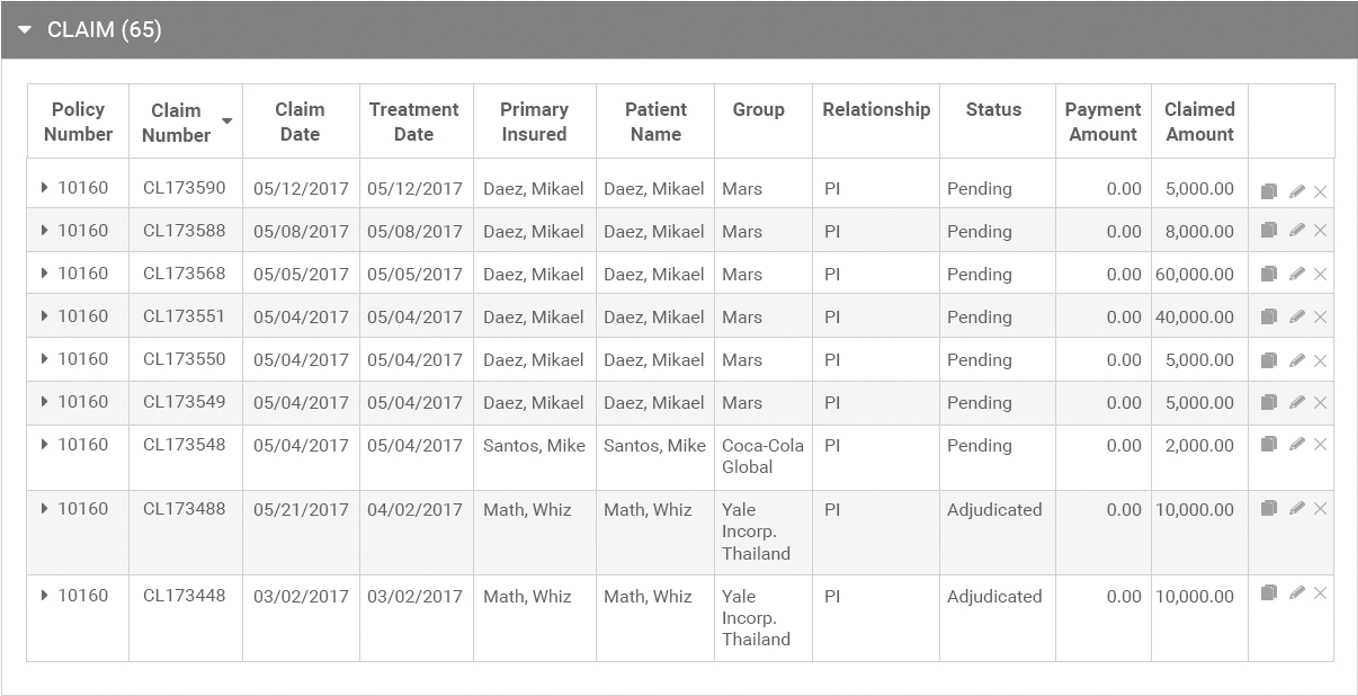
The Claim Types Supported
(Outpatient)
(Inpatient)
(TPD, Life, Trauma)
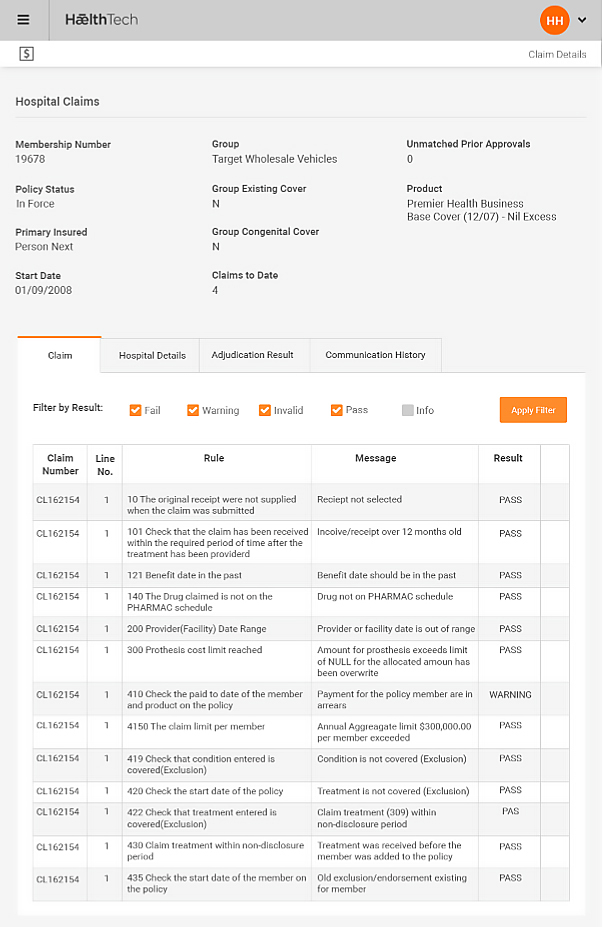
Adjudication
An Intelligent Rules Based Adjudicator
Omni uses an intelligent rules-engine:
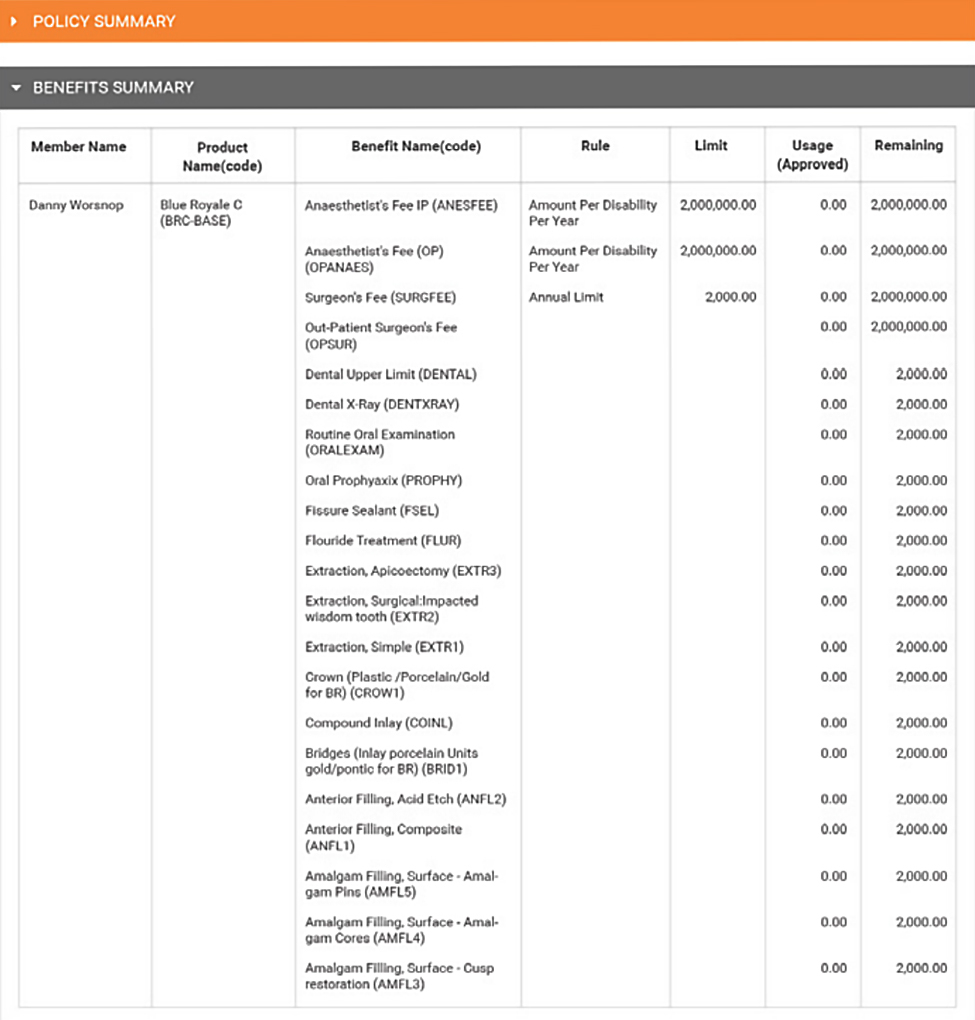
- Identify all policy and underwriting
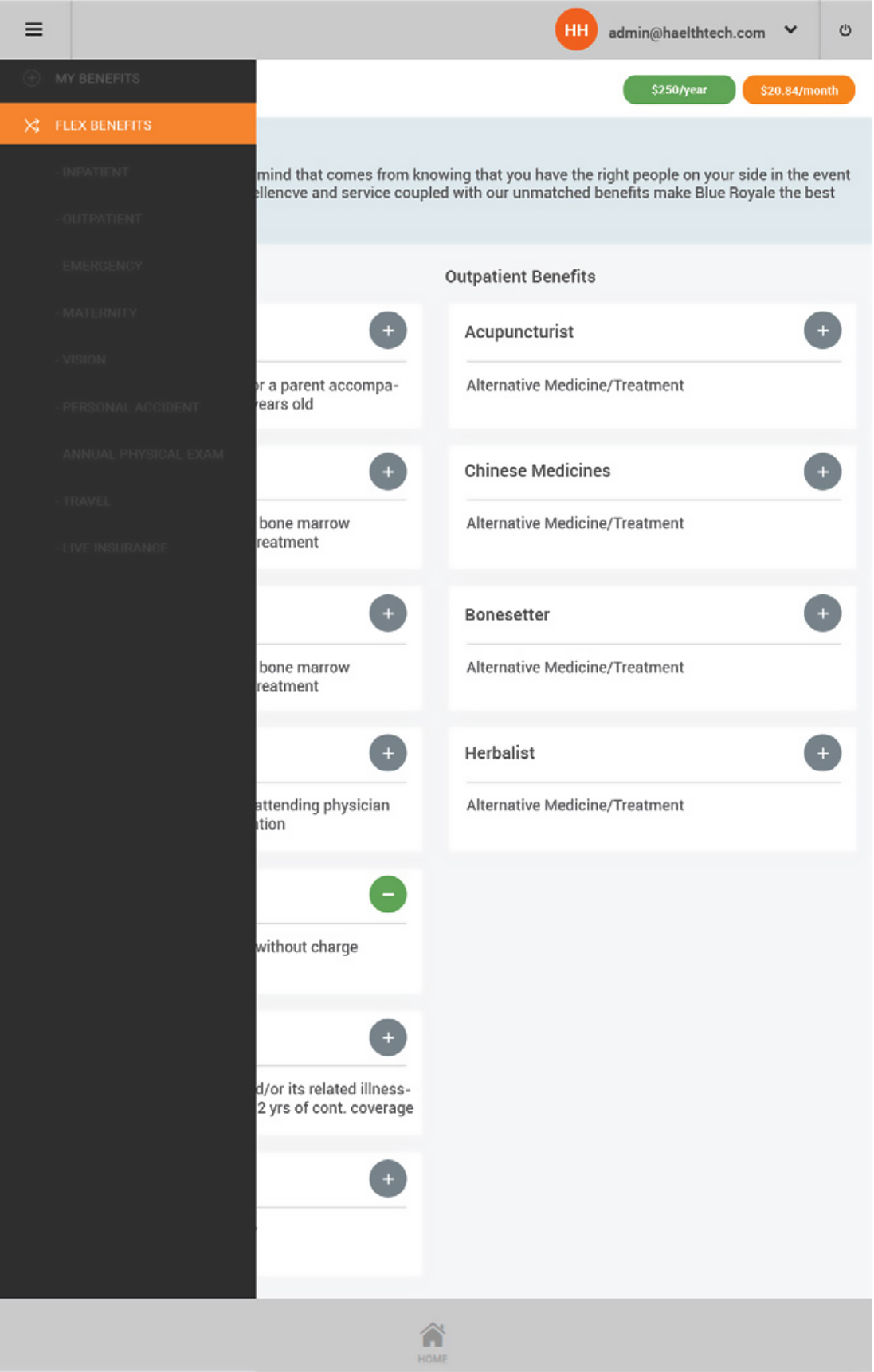
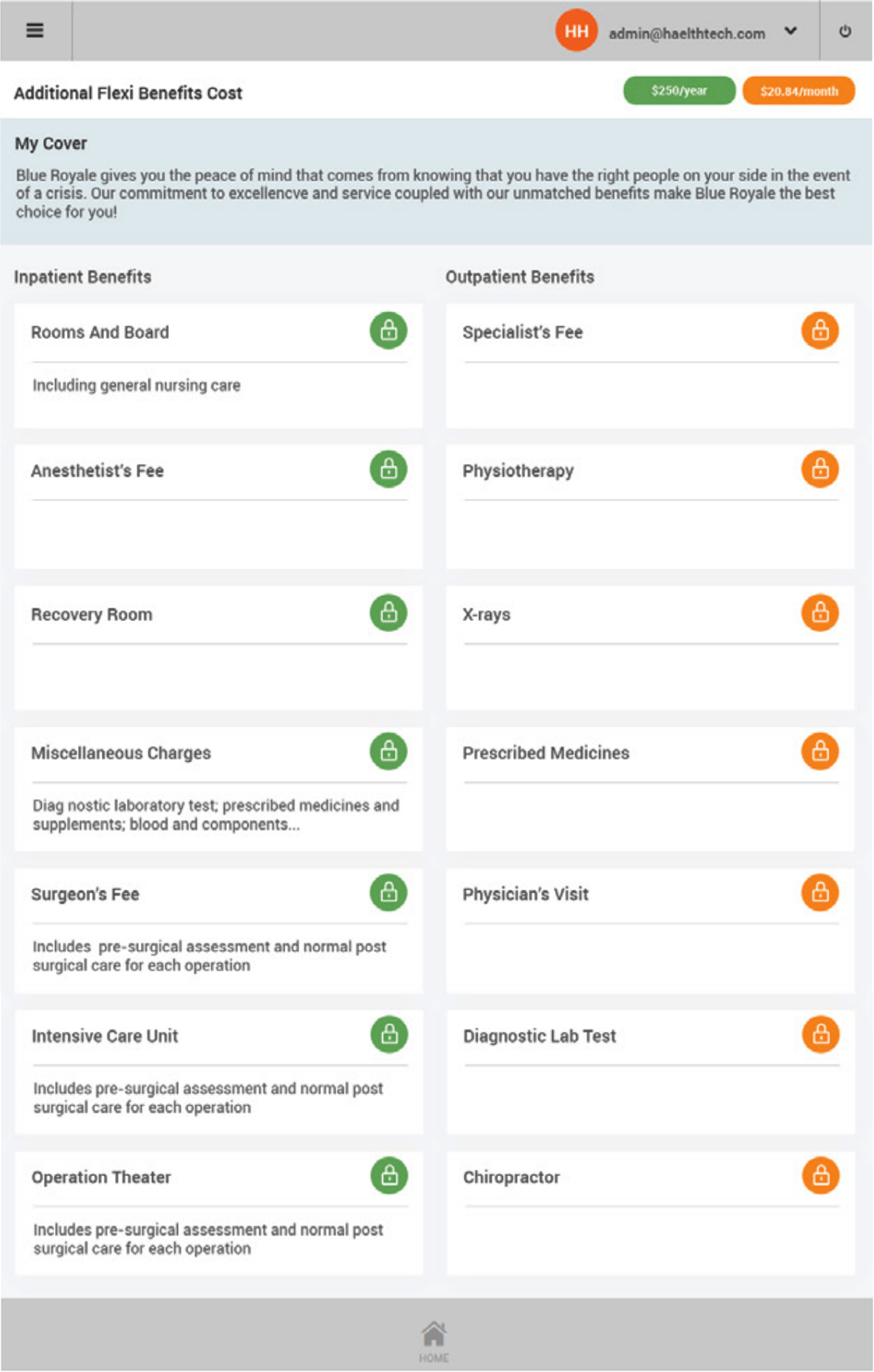
- Identify all products and benefit limits
- Make all pass & fail decisions
- No human intervention or product knowledge required
- Members, providers, TPA’s, HR can enter claims without the need to understand product complexities
- Over 100 pre-defined rules pre-configured for immediate use
The Benefits
Omni uses an intelligent rules-engine:
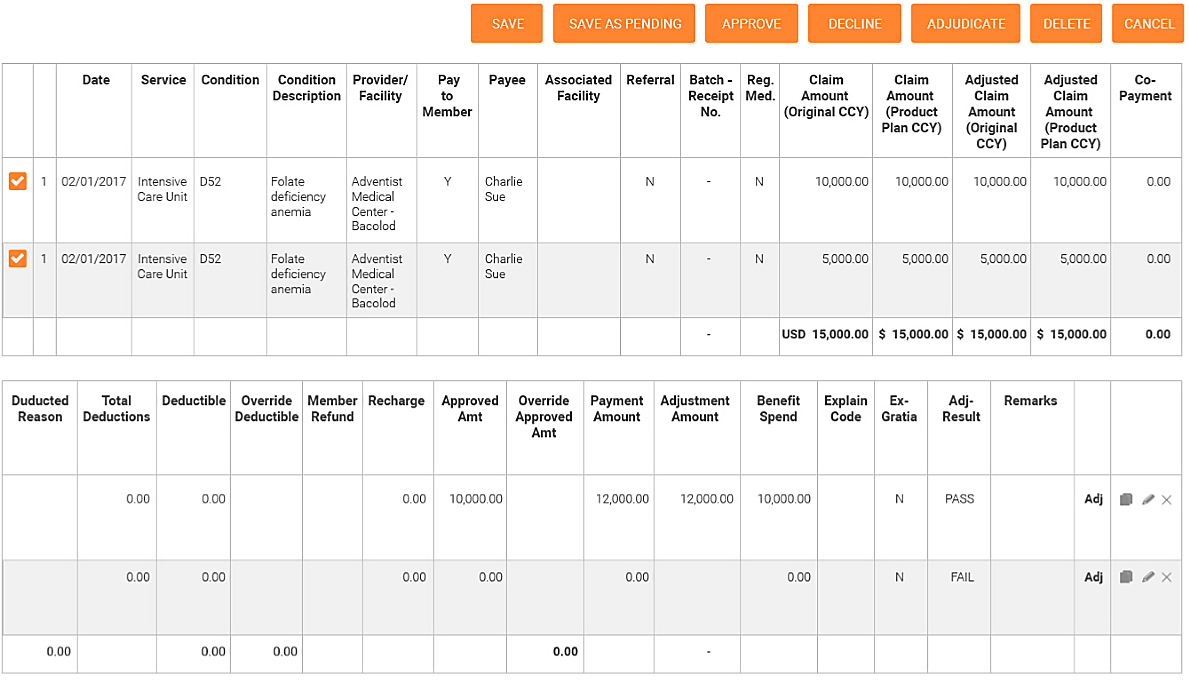
- Complex claims adjudicate in real-time, sub-second
- Greater than 95% of all claims will pass through the adjudication engine without any need for operator intervention
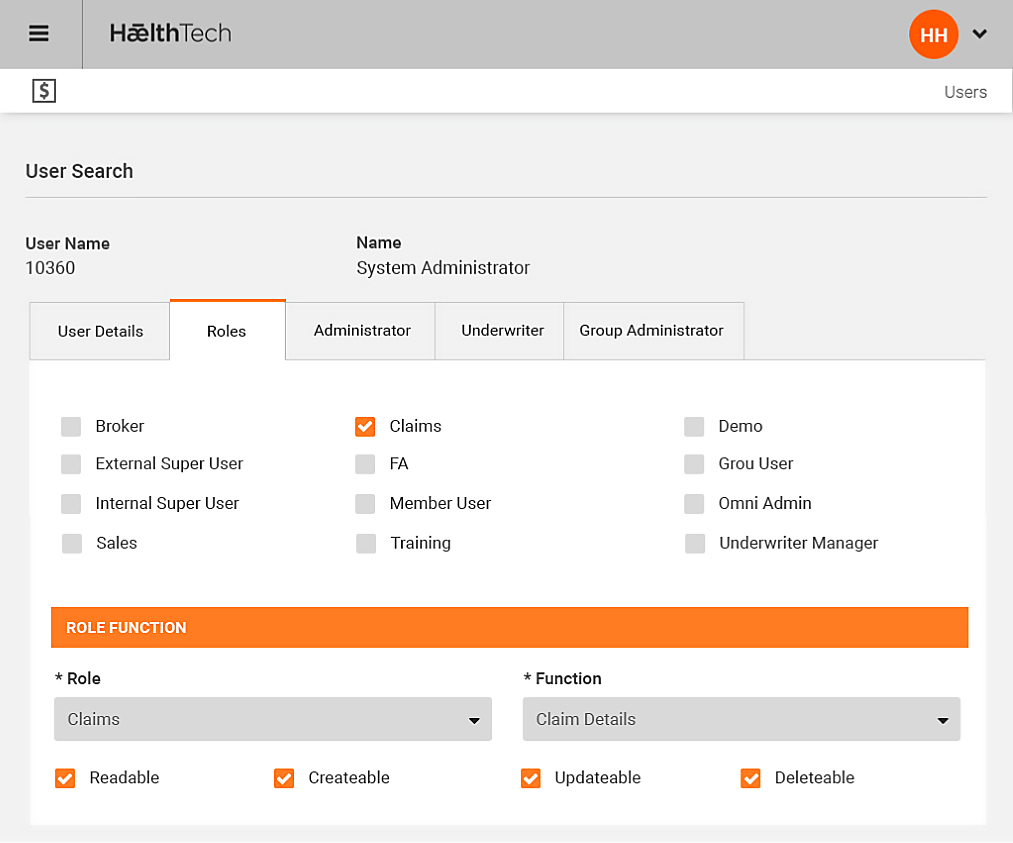
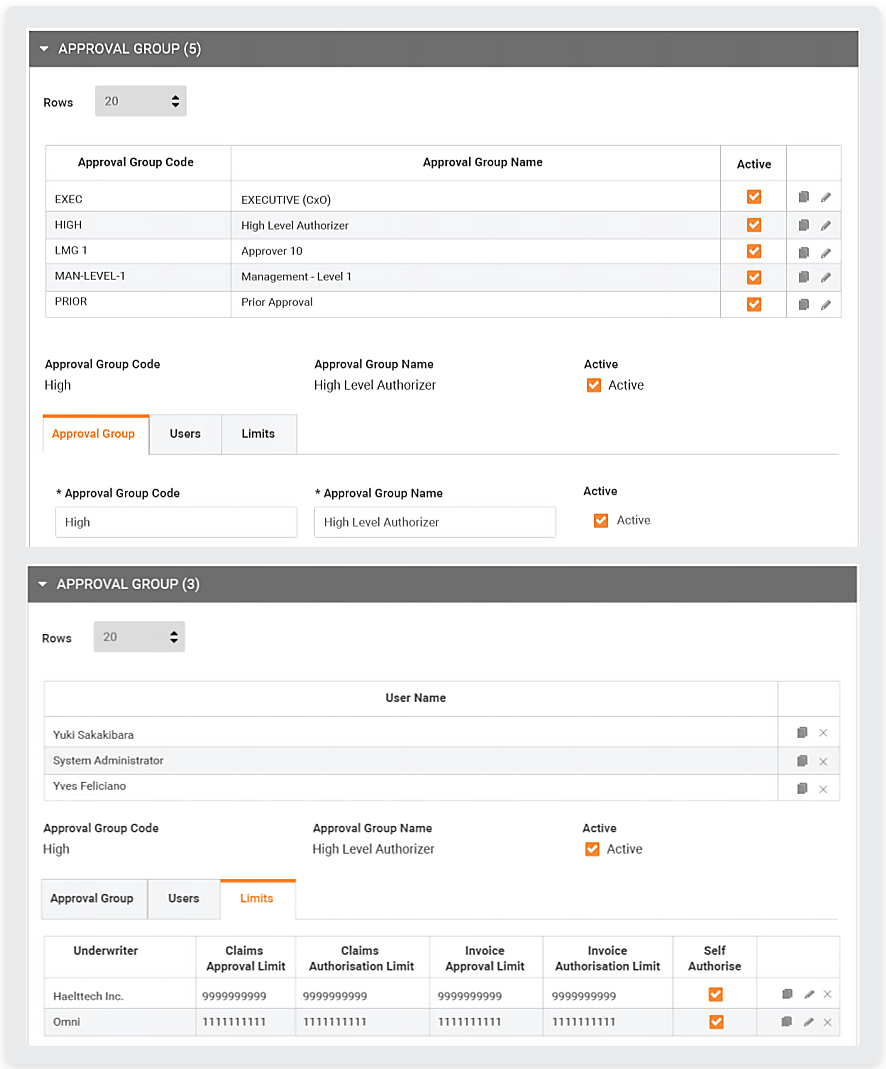
- Omni allows for work-flow based authorisation controls allowing claims to adjudicate and pass for payment or await authorisation by higher user security clearances
- Individual claim lines can be pre-released while the balance of the claim is administered e.g. Paying Specialists before hospitals
- Claims can be paid real-time, or in batch
An Intelligent Rules, more accurately
- Operate with as few as 10% concurrent staff numbers
- Electronic rules adjudication – as many as 40 adjudication checks will be undertaken on each claim line claims - sub-second
- -95% of claims are adjudicated without human intervention
- Self service options allowing providers, groups and members to enter their own claims and have them adjudicated in real time
- Benefit limits & utilisation of benefits are on-line to the adjudication engine to ensure true risk is managed
| Market Observation | Omni |
|---|---|
|
1 administrator per 1,000 members insured |
1 per administrator per 10,000+ members insured |
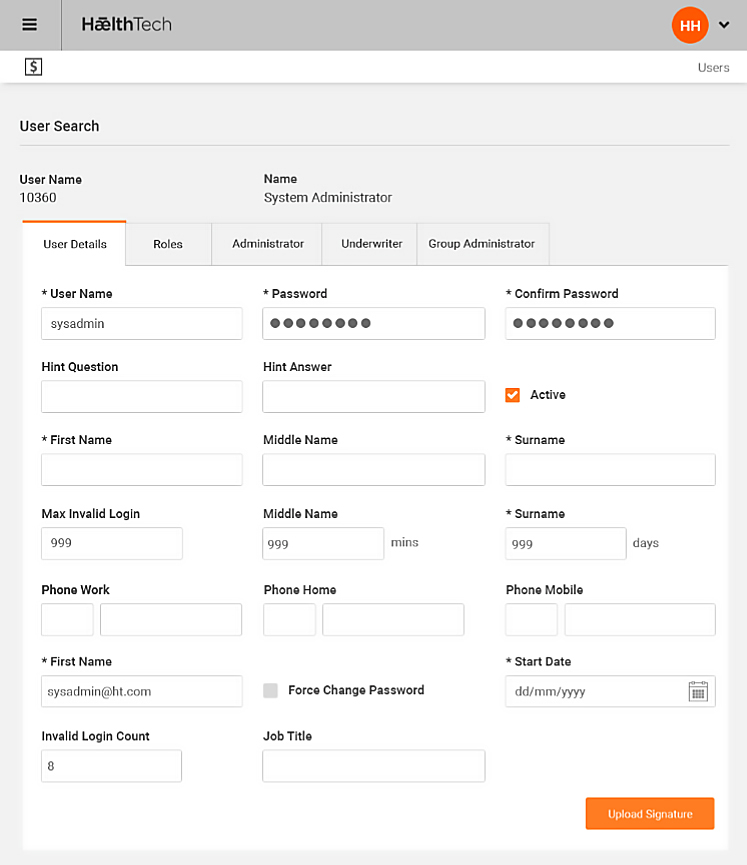
A Secure and Controlled Process
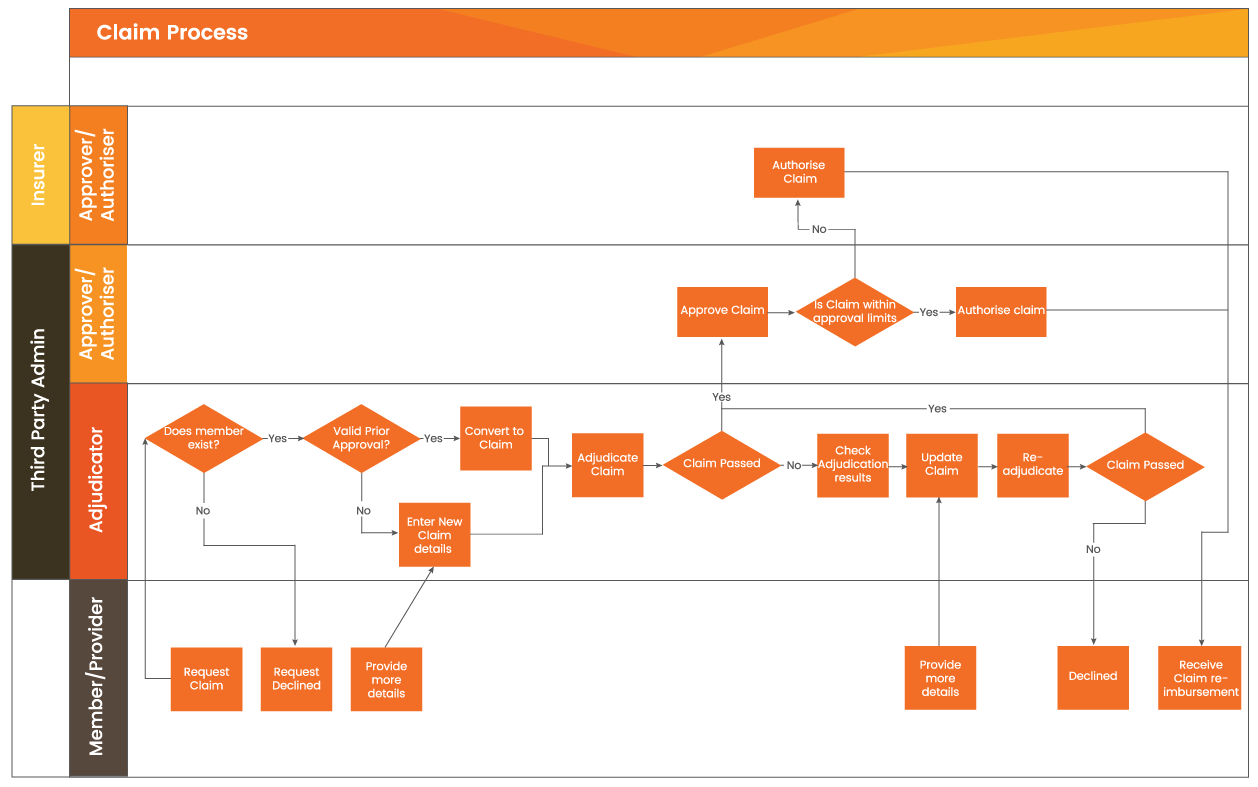
Claims Approval Control
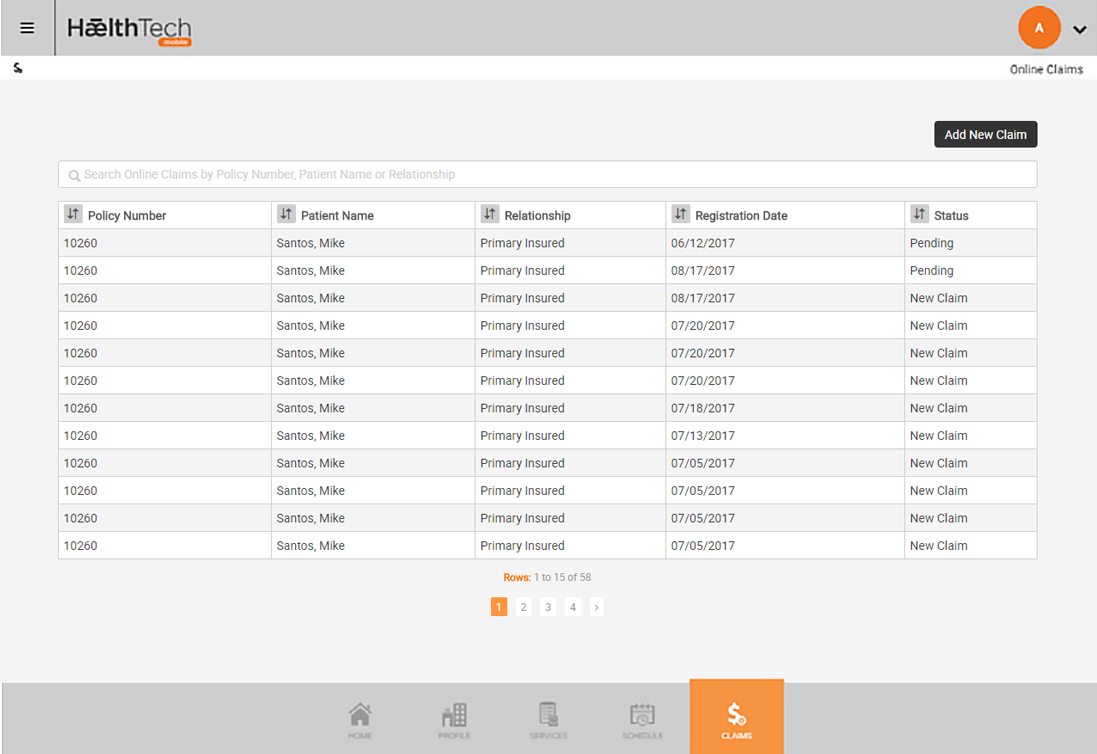
Provider Claims
Provider Claims
A mechanism to connect the providers directly to the Omni administration System by allowing providers to enter claims
Risk Management
Provides access to underwriting rules and adjudication engines within Omni
Efficiencies
Ensures that data is entered once relieving administration overheads
Real Time
Claims can be monitored in real-time by the insurer
TPA
Re-positions that role of the TPA and reduces 3rd party administration cost
Unloads
administration overheads
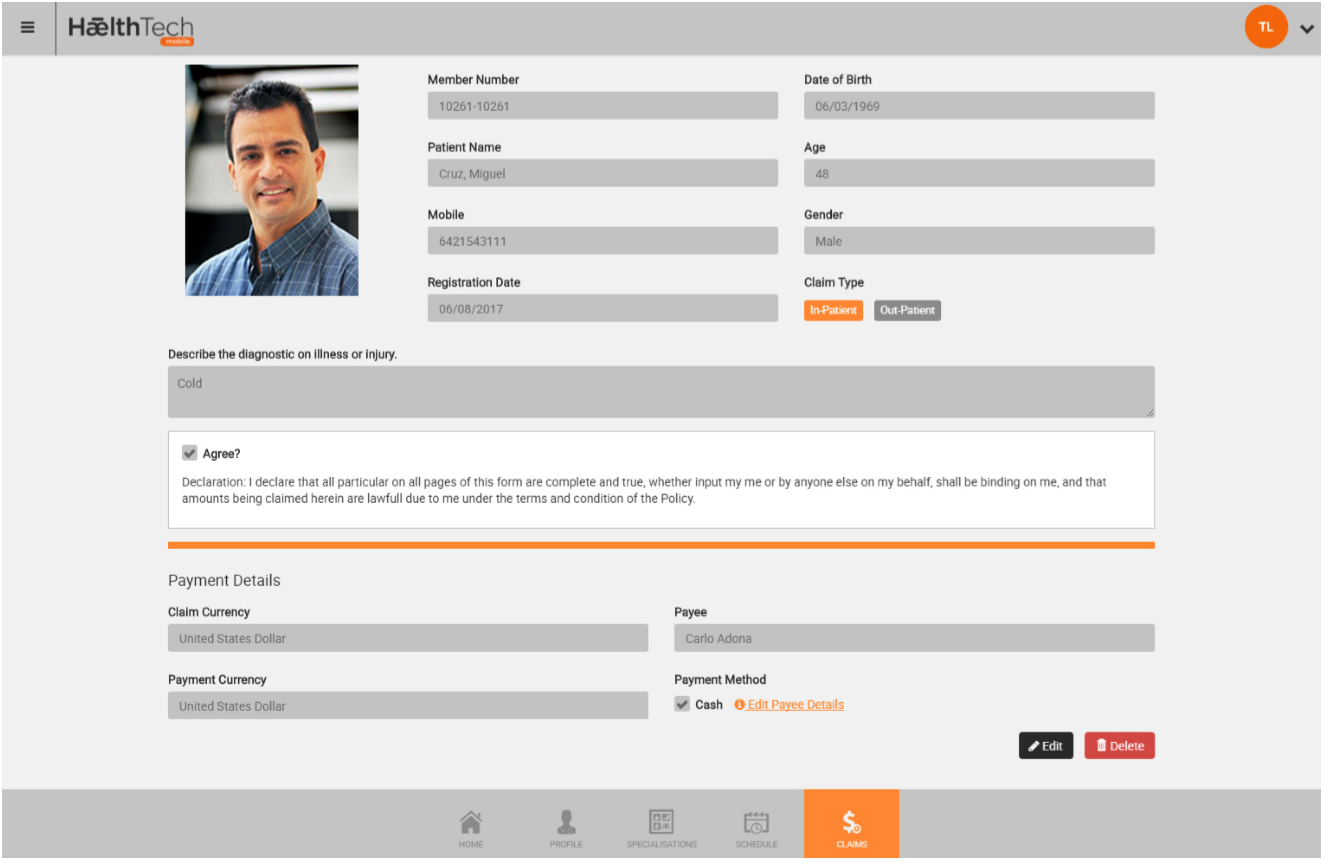
DESIGN
Ideally for In-Network Hospitals and Clinics
Available to providers via mobile devices and the web – directly coupled to the Omni backend administration system including the adjudication engine and all risk management features.
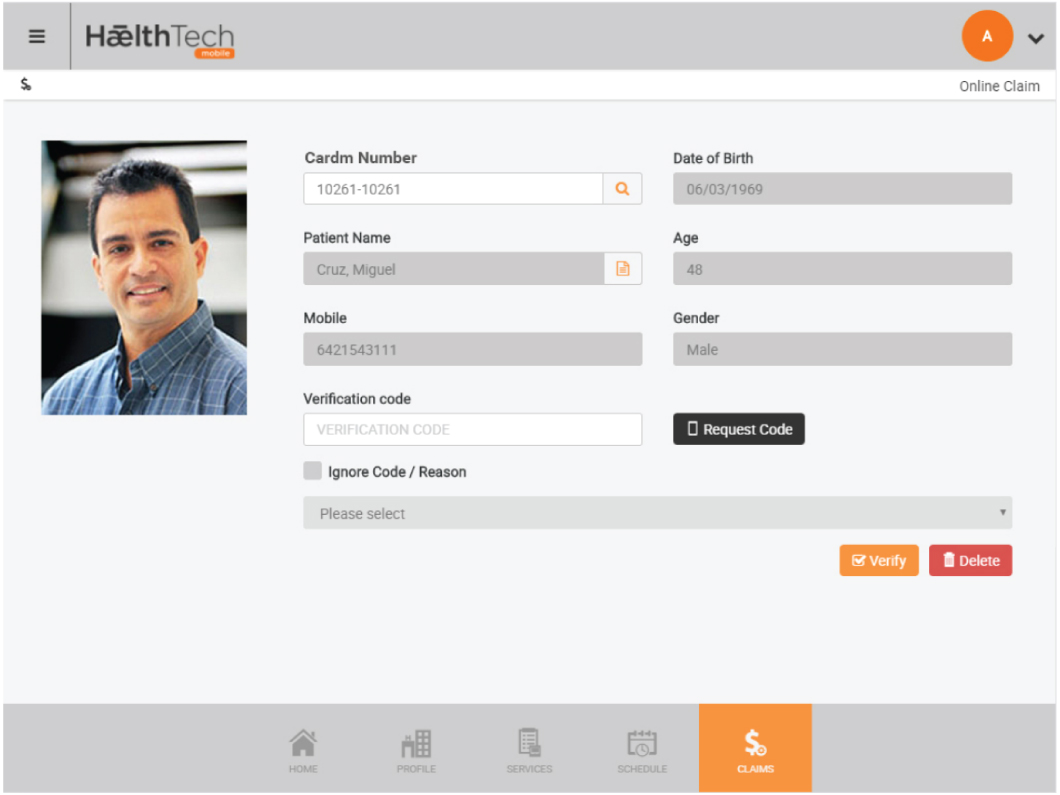
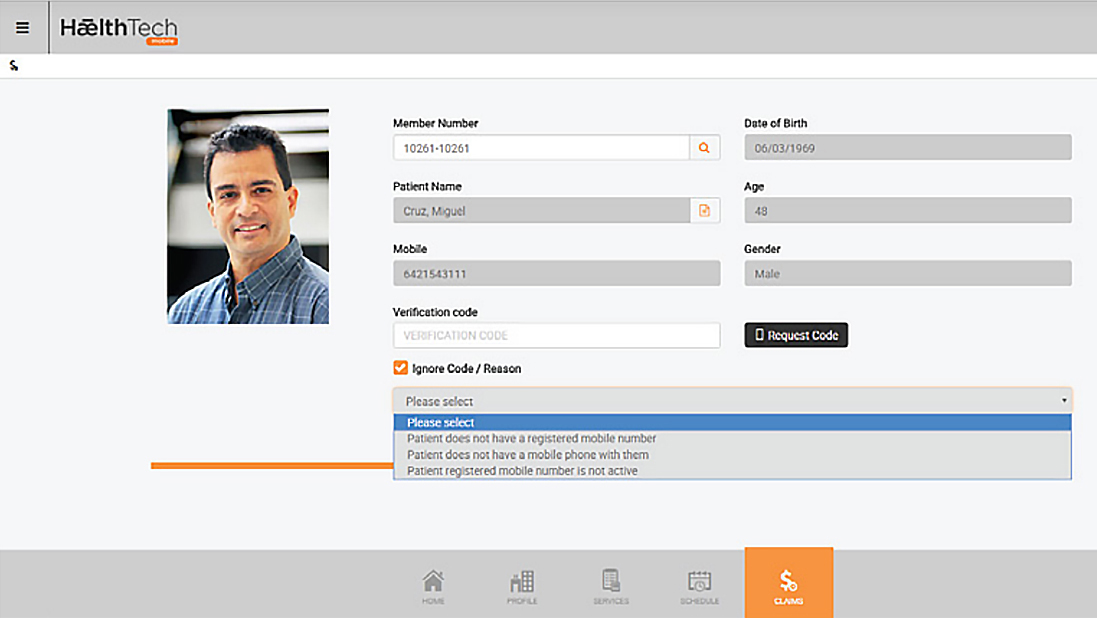
3 Factor Authentication of member–Card number, photo-ID, SMS verification to members phone
Control & management with member Mobility

- Member claims
- In-network provider identification
- Claim status
- Policy & benefit information
- Two Factor Authentication and Photo ID